The protective role of vitamin D in BNT162b2 vaccine-related acute myocarditis
-
An interesting study from China.
The protective role of vitamin D in BNT162b2 vaccine-related acute myocarditis (2025)
Results: A high incidence of hypovitaminosis D (73.3%) was observed in these individuals with vaccine-related myocarditis, particularly in those presented with chest pain or intensive care unit (ICU) admission. Moreover, vitamin D level was negatively associated with peak serum cardiac troponin T level during vaccine-related myocarditis. Genotypically, the GC (vitamin D binding protein) rs4588T allele which encoded the GC2 isoform of vitamin D binding protein was a risk allele, whereas the GC1S isoform was protective. Mechanistically, hypovitaminosis D was associated with higher levels of cytokines pivotal for natural killer (NK) cells (particularly interleukin-1β (IL-1β), IL-12, Interferon-γ (IFN-γ), and IL-8) and higher percentage of CD69+ NK cells in blood, which in turn correlated with chest pain presentation.
Conclusion: These data support the hypothesis that vitamin D plays a crucial role in mitigating mRNA vaccine-related myocarditis by modulating proinflammatory cytokine milieu and subsequent unfavorable NK cell activation, laying a groundwork for preventive and treatment strategies.
-
And from Thailand:
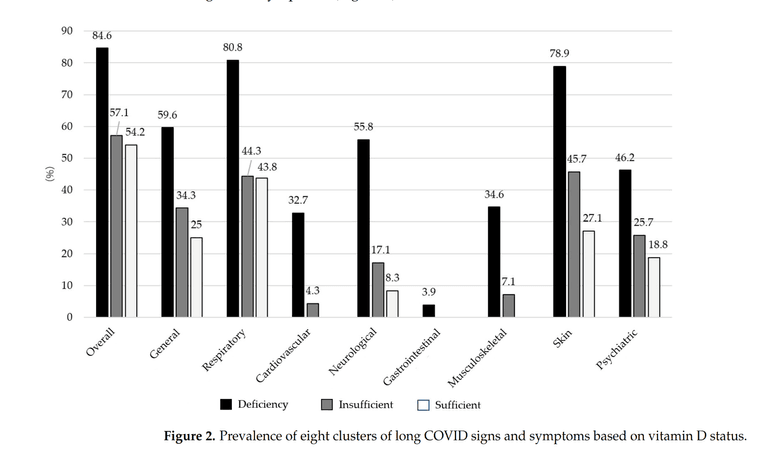
Association Between Vitamin D Levels and Long COVID Signs and Symptoms (2025)Results: The study results indicated a female-to-male ratio of 1.1:1 and a mean age of 45.87 ± 8.65 years; of these, 62.4% received three doses of the COVID-19 vaccine, and 64.7% developed long COVID. The most prevalent signs and symptoms were respiratory (55.3%), skin (50.6%), and general (39.4%). The median blood vitamin D level was 22.96 ng/mL, with 41.2% of subjects having insufficient levels, 30.6% having deficient levels, and 28.2% having sufficient levels. Patients with long COVID had significantly lower vitamin D levels compared with those without long COVID (21.52 ng/mL vs. 25.46 ng/mL; p < 0.05). Multivariable analysis found that vitamin D deficiency was significantly associated with overall long COVID signs and symptoms (Adj. OR, 5.80 [95% CI: 2.10, 16.13]). Additionally, vitamin D deficiency significantly increased the number of long COVID systemic signs and symptoms (Adj. IRR, 3.30 [2.12, 5.12]).
Conclusion: Assessing and maintaining vitamin D levels, vitamin D supplementation, and sunlight exposure in COVID-19 patients can reduce the risk and severity of long-term COVID-19 signs and symptoms.