Understanding Vitamin A metabolism
-
Understanding Vitamin A metabolism
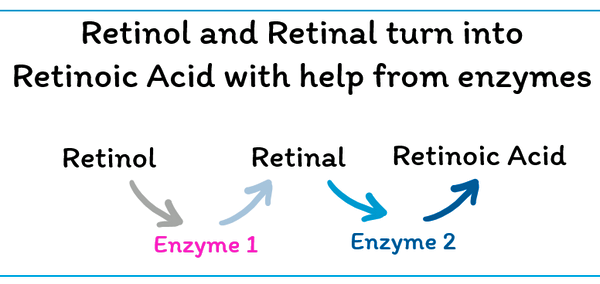
*) The vitamin A pathway
Retinol < = > Retinaldehyde (Aka retinal) → Retinoic acid (aka retinoid)
Absorption and Transport
Fat-soluble vitamin A is absorbed in the small intestine along with dietary fat.
It is transported in the blood as retinol bound to retinol-binding protein (RBP).
In target cells, retinol is converted into various active forms, such as retinoic acid, which is found on nuclear receptors and regulates gene expression.
Vitamin A, in its various forms (retinol and carotenoids), binds thus to specific nuclear receptors called retinoic acid receptors (RARs) and retinoid X receptors (RXRs).
Storage and Regulation
The liver is the primary storage site for vitamin A, where it is esterified and stored as retinyl esters.
The liver also regulates vitamin A levels in the blood by releasing retinol bound to RBP (Retinol Binding Protein). RBP acts as a transport middle.
Specific binding proteins, such as CRBP and CRABP, are involved in the intracellular transport of vitamin A and its derivatives.
InteractionSome intestinal bacteria (commensal bacteria) have the ability to neutralize retinoic receptors in order to lower defense reaction of the immune system. These bacteria create ligands to inactivate the nuclear receptors.
“Any intracellular capable of producing a substance that blocks the VDR would have an effective strategy for disabling the immune system!”
https://mpkb.org/home/pathogenesis/vitamind/metabolism
Excess vitamin A or D - Which ratio is optimal?
Excessive vitamin D intake can lead to vitamin A deficiency through antagonism. Likewise, excess vitamin A can also lead to vitamin A deficiency (if you eat liver > 1x/week or if you ingest 5000 IU / 1500 mcg A1 several times a week).
Explanation: High amounts of vitamin D or vitamin A can interfere with each other's signaling through shared nuclear receptors, primarily the retinoid X receptor (RXR). Both vitamin A (as retinoic acid) and vitamin D (as calcitriol) bind to nuclear receptors, and RXR is a common heterodimer partner for these receptors. This interaction can affect the overall effects of each vitamin on gene expression.
RXR as a Common Partner:
The Vitamin D Receptor (VDR) and the Retinoic Acid Receptors (RARs, which bind retinoic acid) form heterodimers with RXR to regulate gene expression.
Competition for RXR:
When both vitamin A and vitamin D are present in high amounts, they compete for binding to RXR. This can lead to a situation where one vitamin's signaling pathway is favored over the other.
Since RXR proteins are known as partners for some other nuclear receptors (thyroid hormone, liver X), it is possible that due to their common RXR nuclear binding partners, the ligands vitamins D and A antagonize each other’s effects when excess of vitamin A may make vitamin D supplementation less effective.
doi: 10.5114/ceji.2021.103540 Cent Eur J Immunol. 2021
Note: Ray Peat has said we should adapt the amount of vitamin A to the level of our carburation. If we are hypo, we should supplement with lower vitamin A levels. Retinol influences how the body converts T4 (thyroxine) into the active form, T3 (triiodothyronine).
doi: 10.3389/fendo.2022.968215 Front Endocrinol
doi: 10.1007/s00394-022-02945-5 Eur J Nutr. 2022
Vitamin E, as an antioxidant, can help neutralize the damaging effects of excess vitamin A. Vitamin E supplementation was shown to reduce the negative impact of high vitamin A on growth, spleen and testes weight, and adrenal weight. 5 UI vitamin E is enough.
https://doi.org/10.1093/jn/105.12.1600 The Journal of Nutrition 1975
Excerpt: The two effects tend to cancel each other in the sense that the group fed both vitamins A & E had an average relative adrenal weight quite close to that of the group fed only the basal diet. A significant interaction of vitamins A and E was found to effect plasma total protein, liver vitamin A, and relative weight of spleen and testes.Conversion Pathways
Contribution of vitamin A1 to the active form ATRA (All-trans retinoic acid).
Retinol → Retinal → ATRA
Contribution of vitamin A5 to the active form 9CDHRA (9 cis 13,14 dihydro retinoic acid)
9CBC → 9CDHROL → 9CDHRA (usual but not the only conversion pathway). See table.
Contribution of provitamin A (ATBC) to the active form 9CDHRA
9CDHROL → 9CDHRA
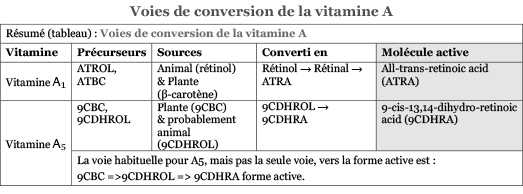
Abbreviations
ATROL all-trans-retinol, forme principale de Vit A1 (vitamine A préformée)
ATBC all-trans beta-carotene
ATRA all-trans retinoic acid
9CBC 9-cis-β,β-carotene
9CDHROL 9-cis-13,14-dihydroretinol
9CDHRA 9-cis-13,14-dihydroretinoic acid -
Optimal dosage of vitamin A
The RDA for vitamin A, expressed as Retinol Activity Equivalents (RAE), is 900 mcg RAE for men and 700 mcg RAE for women. 1300 mcg when pregnant.
While cooked carrots are a good source of Vitamin A (β carotene), when converted to Retinol Activity Equivalents (RAE), the actual usable vitamin A from 100 grams of cooked carrots is significantly less, at 852 micrograms RAE. 852 mcg of which only 10 to 30 % might be absorbed by the body.
When converting plant-based sources of Vitamin A, specifically beta-carotene and 9-cis-beta-carotene (9-CBC), into Retinol Activity Equivalents (RAE), the conversion rates differ. This difference arises because the body's ability to convert different carotenoids into retinol (the active form of Vitamin A) varies. Moreover, individual factors like age, body fat, and genetics can also influence how efficiently carotenoids are converted to retinol.
We could say ~65–80% of vitamin A intake comes from preformed retinol, with the rest from provitamin carotenoids, in countries eating cheese, eggs and drinking milk.
Usual conversion rates: Am J Clin Nutr. 2010. doi: 10.3945/ajcn.2010.28674G (See table 1, “conversion factor”, for conversion rate with fruits & vegetables). Factor 12:1 to 26:1 for orange fruits. 13:1 to 6:1 for sweet potato and spinach.
The body might absorb up to 75% to 100% when preformed retinol is absorbed through food (with some fat) but, in most cases, 10% to 30% when coming via beta-carotene.
https://ods.od.nih.gov/factsheets/VitaminA-HealthProfessional
Conversion rate (Retinol Activity Equivalents (RAE)
RAE is a standardized unit used to express the amount of vitamin A in a food or supplement, taking into account the varying bioavailability of different forms of vitamin A.
For dietary beta-carotene (from food), the conversion is 12 mcg of beta-carotene equals 1 mcg RAE. For beta-carotene from supplements, 6 mcg is equivalent to 1 mcg RAE, according to the Office of Dietary Supplements at NIH.
Simplified ratio: 1 IU retinol = 0.33 mcg RAE.
1 IU dietary beta-carotene = 0.05 mcg RAE.
Note: The conversion rate is very variable, depending on the context, as already pointed. -
Pharmacological dosage of vitamin A as supplement
Inhibitors of retinol
We will assume that we are not dealing with vitamin A inhibitors. Mind when combining 2 or several factors: Alcohol (> 1 glass wine or beer a day), excessive coffee (more than 2-3 cups), cortisone, excess iron (>240; ideal ferritin level at 120 ng/ml), high amount of vegetable oils (> 5 g PUFA), smoking, anti-acid supplement, aspirin 500 mg without making staples (impact on platelets), …
Works synergistically with: Calcium, Phosphorus, Zinc, C, D, E*, Choline, Vitamin B* complex, EFA.- Too much of a good thing is bad.
Optimal range
There is no consensus about the ratio between HD A1 and D3.
Ratio 1:1 to 3:1 for retinol / Vit D3 is optimal when taking a supplement. For Chris Masterjohn
Ratio 4:1 to 8:1 for Dr. Lindsay. More vitamin A than vitamin D. In studies examining the protective effects of cod liver oil against upper respiratory tract infections, Dr. Lindsay and her colleagues used A-to-D ratios between 5:1 and 8:1.
Let’s say we should target 35 ng/mL 25(OH)D levels to limit immune problems. Target 45 ng is optimal
Chris Masterjohn has discussed the importance of maintaining a healthy balance between vitamins A and D, rather than focusing on high levels of either.
• 30 ng/mL as a minimum:
Many experts consider 25(OH)D levels of 30 ng/mL (75 nmol/L) and above to be sufficient for most adults to maintain bone health and potentially reduce the risk of some diseases.
• 40-60 ng/mL for potential benefits:
Some research suggests that higher levels within the 40-60 ng/mL (100-150 nmol/L) range may offer additional benefits, potentially reducing the risk of certain cancers, autoimmune diseases, and other conditions.
Note: When you reach a ceiling below 40 ng/mL Vit D, you must be careful not to exceed 420 mg of elemental magnesium. Has to be confirmed with practical guidance.Optimal vitamin D level
There is some good evidence that 25(OH)D levels should be at least 30-35 ng/ mL (75-88 nmol/L). Much higher levels may be better, or they could start causing harm, especially in the absence of adequate vitamins A and K2. Once we leave the land of 30-35 ng/mL, however, we enter the land of speculation.
Sources:
Chris Masterjohn – Westonprice.org 2010.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8003866Synergism between Vitamin A and Vitamin D but Excess Vitamin A causes Bone Problems
A study from NIH has shown that Vitamin A, specifically retinoic acid (RA), can increase Vitamin D Receptor (VDR) expression by up to 3-fold in certain cell types. This increase is observed in various tissues and cell types, including T cells and muscle cells, when treated with RA. The study also suggests that RA-induced VDR expression can be affected by Vitamin D, and vice versa, highlighting a complex interplay between these two important nutrients.
The dose from research was less than 5000 IU of Vitamin A (1500mcg) that get best benefits.
However, an increased VDR expression due to high level of retinoic acid (RA) can influence the downstream effects of both Vitamin A and Vitamin D signaling pathways.
doi: 10.3389/fimmu.2021.684015 Fatima A H Al-Jaberi et al. 2021. Front Immunol.Interaction and Proposed Ratios
Chris Masterjohn describes a dynamic synergy: Vitamin A and vitamin D each mitigate the other’s toxicity, but when one is excessive relative to the other, metabolic harm may occur—such as bone loss (from too much A alone) or soft tissue calcification (from too much D alone). Vitamin K₂ is essential to activate key Gla proteins like osteocalcin and matrix Gla protein, helping ensure calcium goes into bone rather than soft tissues and articulations.
Source: mountaindogdiet.com interview with Chris Masterjohn: Dynamic synergy between vitamin A and vitamin D.
According to the gosling study (poultry nutrition), overly high A relative to D impaired growth—even moderate A antagonized D at low D levels. Growth was optimized with ratios closer to ~3.5:1 or lower.Addressing Thyroid Status according to Ray Peat Considerations
I’ve noted Ray Peat’s concept of reducing retinoic acid when hypothyroid. In those cases, it may make sense to lean toward a lower A:D ratio, perhaps closer to 1:1, or even shift toward more D if RA synthesis slows. Evidence from community reports aligns: hypothyroid individuals frequently struggle to raise 25(OH)D even with doses alone, but see improvement when vitamin A is added—but only in appropriate ratios.
Thus, especially if hypothyroid, starting with ~1,000 IU A with ~1,000 IU D₃ may be more effective, slowly titrating both up while testing 25(OH)D serum, and watching for signs of imbalance.Adressing the balance for liposoluble vitamins
Talk with ChatGPT. My final target (based on known data), making things reachable
• To reach 35 ng/mL 25(OH)D, ~2,000–3,000 IU D₃/day may be needed for most adults (see meta analysis: European adults ~2,500 IU/d → ~75 nmol/L, i.e. ~30 ng/mL) pubmed.ncbi.nlm.nih.gov.
• To maintain a sane A:D ratio between ~1:1 and 3:1, vitamin A intake at ~2,000–6,000 IU depending on your chosen D dose is reasonable.
• Your 1 mg K₂ MK 4 aligns well with vitamin K needs to activate the Gla proteins.
• Start perhaps with a mid point: 3,000 IU A in morning, 2,500 IU D₃ evening, and keep K₂ midday with fat. Check serum 25(OH)D and adjust.Summary
Chris Masterjohn strongly advocates balanced A:D ratios (~1:1 to 3:1); 5:1 is higher than typical guidance and risks antagonism.
To reach 35 ng/mL D, I likely need 2,000–3,000 IU D daily.
Therefore 2,000–6,000 IU vitamin A, paired with your 1 mg MK‑4, would better align with balance principles.
And if hypothyroid, sticking closer to 1:1 may be safer.
All doses remain below toxicity thresholds (UL for A ≈ 10,000 IU/day; for D ≈ 4,000 IU/day) but we’re in pharmacologic range—monitor labs.
If you want more Vit A, start perhaps with a mid point: 3,000 IU A in morning, 2,500 IU D₃ evening, and keep K₂ midday with fat at 1 mg. Check serum 25(OH)D and adjust.Supporting Chris Masterjohn Sources
• He emphasizes the necessity to balance A and D (synergistic moderation), and cautions that excess of one can poison the other’s benefits; optimal functioning requires balanced intake plus adequate K₂ to activate key proteins
• Balance extra 500 µg K₂ with 3,000 IU A and 900 IU D offers a template to scale up proportionally as doses rise.