Intolerance and Food Hypersensitivity Reactions
-
Intolerance and Food Hypersensitivity Reactions
Intolerance and allergy
We are not talking about celiac disease, the “official” recognized pathology with definite antibodies. In USA and Europe 10 % people are identified as suffering from gluten disorder. 5-10 % more are supposed not to have been well identified (undiagnosed or misdiagnosed). One third of which could suffer from a cross-reaction with other peptides (proteins from milk products or other sources). I’m not talking here about gas and flatulence when drinking one liter milk (2.2 Lbs.) because you’ve exhausted lactase enzymes.
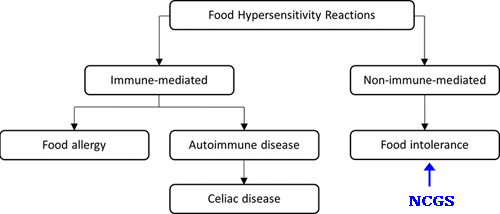
Differential diagnose hard to settle
I mentioned 10 % identified but the admitted official amount is 1.26% (1) for confirmed patients suffering from a well-defined autoimmune disorder. Though a differential diagnose could be hard to settle, NCGS symptoms can overlap with other gastrointestinal conditions.
NCGS = Non-Celiac Gluten Sensitivity
Celiac and non-celiac
Symptoms of both conditions can include abdominal pain, bloating, flatulence, diarrhea and other gastrointestinal issues.
Self-reported NCWS was found to be common in Italian teenagers, with a frequency of 12.2%; the frequency of GFD use was 2.9%, which was much higher than the percentage of known CD in the same population (1.26%). (2)
NCWS = Non-Celiac Wheat Sensitivity
GFD = gluten-free diet
GD = gluten disorder
In NCGS, these symptoms improve when gluten is removed from the diet, but there is no autoimmune response or intestinal damage characteristic of celiac disease.
Therefore, the question is not about celiac disease, but about the possibility of another condition, NCGS, that can cause similar digestive problems.
Permeability of the border brush of the intestines (villi)
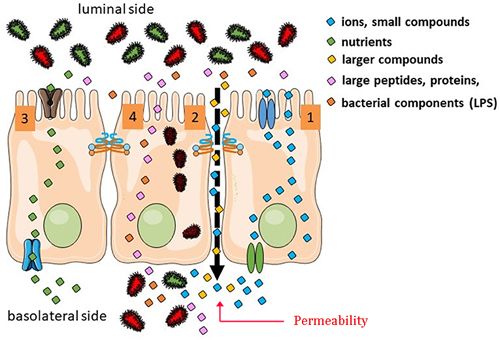
When consuming wheat from bread, pasta, pastry or biscuits – and other less problematic peptides from milk products or corn – we act on the zonulin. Zonulin is a protein that regulates tight junctions. Zonulin regulates tight junctions between cells in the intestinal wall, thus controlling the passage of substances across the intestinal barrier.
Note: The impact is real for everybody, with or without noticeable reaction. The degree of enlargement being different, then. When we have over-extended the rope (frequency), we are likely to suffer from low-grade inflammation. This means that most people will not notice / record significant disturbances. Under the radar then.
For most of us – let’s say 80 % – we’ll recover during the night, unaware of the situation. For the other 15-20 %, these persons would most likely suffer from ongoing digestive symptoms, yet don’t realize gluten (or something else in their diet) might be contributing — and that they could potentially improve if they identified and adjusted their habits.
Figure: Reaction to peptides from different foods
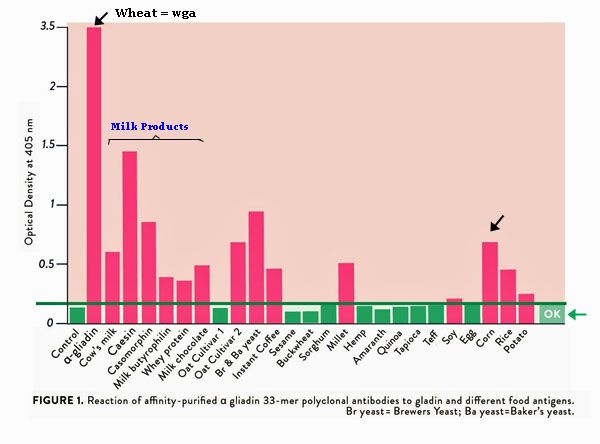
Source: The Paleo Mom – Gluten Cross-Reactivity
Credit: DOI: 10.4236/fns.2013.41005
Food and Nutrition Sciences. January 2013. Aristo Vojdani, Igal Tarash.
Gut repair
Gut repair during the night is facilitated by a combination of factors, including the body's natural autophagy process, which is most active during sleep, and the support of certain foods and supplements. Prioritizing sleep, managing stress, and adopting a balanced diet can further enhance this process.
How Gut Repair Works at Night (if you digest well)
• Autophagy
During sleep, the body engages in cellular repair, including in the gut, through a process called autophagy. This process helps remove damaged cells and debris, promoting overall gut health.
• Digestive Rest
While the gut's activity slows down at night, this allows for a period of rest and recovery, potentially preserving a healthy gut lining.
• Support
Focus at the evening meal on consuming foods rich in probiotics, prebiotics, and specific nutrients like glutamine, zinc, magnesium, and omega-3 fatty acids. These nutrients support the gut lining, reduce inflammation, and aid in the growth of beneficial bacteria. Mind the ratio W6/W3 (ratio 1/1 to 4/1 when trying to heal. But with a very moderate amount (5 g fat) since PUFA are very fragile (rapidly oxidized and / or incorporated in AA cascade).
Note: No prebiotic if you suffer from dysbiosis. Not the right time. When taking glutamine (half tsp powder), some taurine is required to normalize possible glutamate excitoxicity.Sources and references
- Self-Reported Non-Celiac Wheat Sensitivity in High School Students: Demographic and Clinical Characteristics. Nutrients. 2017 Jul. https://doi.org/10.3390/nu9070771
- Suspected Non-celiac Gluten Sensitivity Confirmed in Few Patients after Gluten Challenge in Double-Blind, Placebo-Controlled Trials
DOI: 10.1016/j.cgh.2016.08.007
16% NCGS patients showed gluten-specific symptoms in 10 double-blind, placebo-controlled, gluten-challenge trials, comprising 1312 adults. 2027 Clin Gastroenterol Hepatol. - The role of zonulin in intestinal permeability (leaky gut)
https://www.assaygenie.com/blog/zonulin-intestinal-permeability#:~:text=What is Zonulin and where,legumes%2C nuts%2C and seeds.
Key Takeaways:
- Zonulin is a protein regulating intestinal permeability, or "leaky gut."
- It modulates tight junctions in the intestines, affecting substance passage into the bloodstream.
- Dysregulated zonulin levels are linked to autoimmune disorders, celiac disease, diabetes, and Alzheimer's.
- Zonulin is involved in diseases like Crohn's and cancer, and its inhibitors are being researched.
- Elevated zonulin levels can increase bacterial adhesion and intestinal permeability.
- Intolerance and food hypersensitivity reactions
More details on this post (with links):
https://mirzoune-ciboulette.forumactif.org/t2123-english-corner-intolerance-and-food-hypersensitivity-reactions#30280