Why is the epidemiological literature overwhelmingly in favor of PUFAs?
-
In pretty much every retrospective, cohort study or RCT I happen to take a look at, higher PUFA consumption, especially linoleic acid, almost always leads to better outcomes than lower PUFA consumption.
Example of a study I came upon by chance: https://pubmed.ncbi.nlm.nih.gov/35170737/
Higher n-6 PUFA consumption cuts the risk of dying by half in newly diagnosed head/neck cancer patients.
Example 2:
https://pubmed.ncbi.nlm.nih.gov/34434952/Highest vs lowest PUFA quartile associated with 20% decreased all-cause mortality
Is healthy user bias enough to explain this?
-
-
And yet in real life, the more of these you consume, the worse off you are
-
@skylark How are the examples I provided not "real life"?
-
@Vapid-Bobcat This is what the conclusion of the study you posted says btw:
During the study period, there were 115 recurrent and 211 death events. High LCFA intake was associated with a reduced all-cause mortality risk (HR: 0.55; 95% CI: 0.34, 0.91; P-trend = 0.02). High unsaturated FA intake was associated with a reduced all-cause mortality risk (HR: 0.62; 95% CI: 0.40, 0.97; P-trend = 0.04) and HNSCC-specific mortality risk (HR: 0.51; 95% CI: 0.29, 0.90; P-trend = 0.02). High intakes of ω-3 PUFAs (HR: 0.56; 95% CI: 0.35, 0.91; P-trend = 0.02) and ω-6 PUFAs (HR: 0.57; 95% CI: 0.34, 0.94; P-trend = 0.02) were significantly associated with a reduced all-cause mortality risk. There were no significant associations between other fat types and recurrence or mortality risk.
-
@thyroidchor27 I read the conclusion, obviously. What are you trying to state?
-
@Vapid-Bobcat I think the answer is that both PUFA and SFA are beneficial. I’d be curious as to what the dose of PUFA is that’s considered beneficial. The issue might be the demonization of saturated fat, rather than PUFA’s specifically in themselves. Maybe something like a Saturated/Mono/Poly split of 45/40/15. I think this also explain taste preferences. Coconut oil doesn’t really hit the same as butter, steak, pork fat, chicken skin, etc.
-
@dan-saintdominic Isn't PUFA being the scourge of the modern diet a main tenet of the Ray Peat philosohpy?
-
@Vapid-Bobcat Yes that’s his proposition.
-
Good question!
Epidemiological literature is tainted heavily with healthy and unhealthy user biases, risk-taking behavior, people lying on surveys, etc. It's a very low-level of understanding for how xyz effects something. You also have to look at what they are measuring, especially with RCTS where they'll take triglycerides or LDL as indications of cardiac risk. With this, they'll say that a reduction in cholesterol means you are healthier and less at-risk but, in fact, you're cholesterol is down due to liver damage from omega-6 and in the long-term you're at a higher risk of dying- though you'll be indistinguishable in risk from someone eating high saturated fat and regularly smoking.
As to the studies you cited:
Your cancer study has quite some interesting data and the authors have some interesting things to say.
-
The study shows that moderate consumption of PUFA significantly raises all-cause mortality risk and carcinoma–specific mortality risk(1.32 & 1.41, respectively, and far higher than saturated fat risk). Only with high PUFA consumption did the mortality risks decrease(and quite a lot at that!), which would imply that there's bias in reporting or bias in high vs mod PUFA users. The authors partially control from smoking and drinking but admit that their categories are not enough to fully capture the effects.
-
The authors make the point: "Our findings that high intakes of ω-6 PUFAs were associated with a reduced risk of all-cause mortality were inconsistent with other studies that considered that overconsumption of ω-6 PUFAs, which are found in non–marine oil–rich diets, and an increased proportion of the ω-6/ω-3 PUFA ratio promote carcinogenesis by activating inflammation and the production of reactive oxygen species"
The authors make an attempt to obfuscate this inconsistency by saying that it's possibly due to "chance," but it's actually that they did a good job assessing mortality risk but are trapped in a pro-omega 6 paradigm. They actually say "the results might be due to chance because this is an observational study, and we can only determine associations and not causation." Wink wink, it's not chance.
Your other study is quite interesting as well
-
The authors admit that there's no causal inference capable from the observational nature of the study- that's very important.
-
They state that their assessment is based off of a single questionnaire given to people and they do not track whether diets changed over time.
In short, there's a lot of data attached to the study but it's not good data and you cannot make any causal inference from it.
There's a technique in biological statistics called "Mendelian Randomization"(which means that we can look at genetic variations and outcomes of observational studies rather than do controlled trials- a high level of accuracy as to causality and a significant reduction in unmeasured or improperly measured confounding factors). It's perhaps not "Peaty" but Mendelian Randomization is a great development towards dealing with observational data biases and causal inference.
Here's a meta-analysis of RCTS that does a Mendelian Randomization in order to test effects of omega-6 PUFA and cardiovascular disease(CVD). I will add that the study references many other meta-analyses which show variable effects from saturated fat and omega-6 PUFA; these meta-analyses are mostly observational data or RCT analyses with cholesterol biomarkers as indicators of health.
In contrast to the results of the RCT and observational/cohort studies, the MR approach found increases in risk of myocardial infarction(heart attack), stroke, artery stroke, heart disease. Interestingly, the authors also see elevated LDL and HDL cholesterols with increased PUFA, which would indicate under "cholesterol-heart" theory that omega-6 PUFA is good for you, but we know that omega-6 intake elevates endotoxin and cholesterol is used by the body to bind and protect itself from endotoxins in the bloodstream- the increased omega-6 PUFA is increasing cholesterol and risk because it is increasing endotoxins in the body.
In short, you ask a good question and the answer is that epidemiological literature is an incomplete look at mortality and nutrition. It is important to account for influential confounding factors, user bias, as well as advancements in assessing causal relations through statistics.
-
-
@JulofEnoch Thanks for the elaborate answer. I will focus on the second study since it's more general.
I agree that food frecuency questionnaries are extremely limited, but they should probably be good enough to at least discriminate between those at the highest vs lowest perecentiles of PUFA intake.
By its very nature, I doubt MR is a valid way to assess the impact of dietary exposures. Serum omega 6 is not the same as tissue omega-6, and high omega-6 intake doesn't always lead to high serum omega-6.
We know that observational epidemiology cannot make causal inferences, but one has to wonder why high PUFAs, if they truly are the problem Ray Peat outlines them to be, rarely associate with worse health outcomes.
I agree that healthy user bias is probably explaining part or maybe all of the effect of PUFAs on different outcomes. Another possible explanation is over-adjustment for variables such as BMI.
But I still wonder if Peat or the community have found better explanations.
-
I have no disagreements with you on the questionnaires. When I say single, I mean that there was a single instance of data collection, not that only one type of questionnaire was used. We do not know the real long-term composition of people's diets- we have a single snapshot of their diets from a single filling out of a questionnaire.
You are correct that serum =/= tissue, but if you're going to use that against the study you'd need to provide some evidence that there's a sufficient(model invalidating) and widespread enough(population %) gap in PUFA intake to serum levels.
Adrenic acid is formed from linoleic acid or arachidonic acid(which itself is a successor molecule to linoleic acid)- the increased consumption of either would increase AA in the serum, unless you are someone whose tissues are oxidizing PUFA at such a high rate that it cannot accumulate and is almost immediately taken out of the bloodstream.
Speaking for myself, I have my own thoughts regarding things like PUFA and do not think that it's as much an issue for people who are otherwise healthy- barring excessive intakes, terrible 3/6 ratio, and some other things. For me, this comes from experience with medicine and some studies on the impact of behavioral patterns. About 90% of the reduction in CVD risk is behavioral, not dietary or medical. This is a figure that the study finds in its risk data and it's about what I've seen myself.
We know that observational epidemiology cannot make causal inferences, but one has to wonder why high PUFAs, if they truly are the problem Ray Peat outlines them to be, rarely associate with worse health outcomes.
You are seeing them rarely associate within contexts that are not 1 to 1 of PUFA to negative outcomes.
You can torture the PUFA intake variable to control for a vast litany of confounds(like health behaviors, smoking, etc.) but when you do that you need to ask "how many people are we comparing." It's not enough to say that you've controlled for the variables; if we know that increased risky health behaviors are related to increased saturated fat intake, then the number of people we're doing statistical assessments on is likely very low, when we're looking at high saturated fat intake people who do not engage in risky health behaviors.
You're already taking away 90% of the predictive ability regarding CVD when you do behavior controls, so you're left with a limited predictive variable and and limited sample to run tests on. I am not able to find these figures in your study and I don't want to dismiss it by assuming that the study has these issues, but it's something that I would consider in whether you should draw causal evidence from it.
Even Ray Peat said that someone could have a high PUFA intake(he uses PNW natives and Salmon as an example) and be very healthy due to a high rate of PUFA oxidation- the PUFAs don't store. Controlling for health in saturated fat vs PUFA isn't really going to reveal much except that healthy people are healthy.
You're also removing the possibility that increased PUFA consumption does have negative secondary effects like reduced cognition- making someone more susceptible to increased smoking and drinking(which would lead to reduced health outcomes), but when you control for all of the variables you remove the observation of those secondary effects and are thereby isolating PUFAs impact on health in a way which is not found in the real world.
In short, you are lowering the PUFA effects by removing the analysis of secondary effects from increased PUFA consumption as part of model creation.
We do not live in a world where everyone is healthy- people are under the influence of many metabolic stressors and as such PUFA is going to store, oxidize, and interact with deficiencies in order to create obesity, cancer, diabetes, heart disease, alzheimer's, etc.
If we could live in a world where we've made everyone have strong pro-health behaviors, no metabolic stressors, etc. then we'd be able to have a bigger conversation about the proportion of PUFA in the diet and how it relates to heart disease.
Ray's work is about real people in the real world, not people in a model with a dozen variables controlled for in comparison to others. Outside of the controlled variable models, PUFA consumption is not something that we should encourage people to increase, especially because in people who are already sick it will only make them sicker; the same is true of exercise and sick people- exercise does not help but hinders health(mostly by increasing fatty acid oxidation and stress).
I agree that healthy user bias is probably explaining part or maybe all of the effect of PUFAs on different outcomes. Another possible explanation is over-adjustment for variables such as BMI.
It's lazy to say "healthy user bias". There's unhealthy user bias, as well. There's also underreporting of cigarette and alcohol consumption(especially by current and former smokers and heavy drinkers, respectively) which was an issue in the 90s to 2000s(the time period btw that your study gets its data from). This isn't minor underreporting but on the order of 30-40% for cigarettes.
Underreported alcohol intake is most severe with spirits or hard liquor(one study finding two-thirds underreporting), spirits are also the preferred drink of heavy drinkers which adds significant potential for confounding.This confounding is only boosted by the relationship between bad health behaviors like smoking and drinking and the consumption of saturated fat. In the US(at least) these behaviors are often closely related; as such, heavy drinkers who have high saturated fat intake may underreport spirit consumption significantly more than heavy drinkers with high PUFA intake, on account of a strong relationship between diet and bad health behaviors.
This is getting long but it's been good mental exercise for me and I hope it's somewhat informative for you, as well.
One last point to consider is the underreporting of energy intake. Obviously, the groups most likely to consume saturated fat, drink, and smoke, are also most likely to underreport their caloric intake- there's a few studies showing this. If there's non-even distribution of calorie underreporting, you're going to have effects in your model that are non-evenly distributed and that would otherwise not exist in a real 1-to-1 calorie comparison. You would see a statistically-significant association with saturated fat and negative outcomes(and the contrary association of PUFA and positive outcomes) within a controlled-variable model when that association is actually non-existent or even reversed but there's a hidden caloric intake on the side of the unhealthy people- an invisible finger pushing down on the scale within the model. Controlling for variables doesn't mean much when you cannot accurately control them because people are giving you bad data.
-
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10321214/
"Inflammatory bowel disease (IBD) is a multifactorial disease with increasing incidence in the U.S. suggesting that environmental factors, including diet, are involved. It has been suggested that excessive consumption of linoleic acid (LA, C18:2 omega-6), which must be obtained from the diet, may promote the development of IBD in humans. To demonstrate a causal link between LA and IBD, we show that a high fat diet (HFD) based on soybean oil (SO), which is comprised of ~55% LA, increases susceptibility to colitis in several models, including IBD-susceptible IL10 knockout mice. This effect was not observed with low-LA HFDs derived from genetically modified soybean oil or olive oil. The conventional SO HFD causes classical IBD symptoms including immune dysfunction, increased intestinal epithelial barrier permeability, and disruption of the balance of isoforms from the IBD susceptibility gene Hepatocyte Nuclear Factor 4α (HNF4α). The SO HFD causes gut dysbiosis, including increased abundance of an endogenous adherent invasive Escherichia coli (AIEC), which can use LA as a carbon source. Metabolomic analysis shows that in the mouse gut, even in the absence of bacteria, the presence of soybean oil increases levels of LA, oxylipins and prostaglandins. Many compounds in the endocannabinoid system, which are protective against IBD, are decreased by SO both in vivo and in vitro. These results indicate that a high LA diet increases susceptibility to colitis via microbial and host-initiated pathways involving alterations in the balance of bioactive metabolites of omega-6 and omega-3 polyunsaturated fatty acids, as well as HNF4α isoforms."
So genetically removing PUFA from soybean oil, prevents IBD. Omega-6 is a carbon source for adherent invasive Escherichia coli. Another study found that this bacteria can cause Parkinson:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10730176/
"Markedly, the relative abundance of E. coli in the LRRK2+/sPD+ group was almost seven times higher than that in the LRRK2+/sPD- group."So people with a genetic risk variant of Parkinson's (a gene that is involved in the intestinal epithelial barrier), but who don't get Parkinson, have 7 times lower levels of E. coli.
"Animal experiments showed that E. coli administration triggered pathological α-syn accumulation in the colon and spread to the brain via the gut-brain axis in Lrrk2 R1628P mice, due to the co-occurrence of Lrrk2 variant-induced inhibition of α-syn autophagic degradation and increased phosphorylation of α-syn caused by curli in E. coli-derived extracellular vesicles. Fecal microbiota transplantation (FMT) effectively ameliorated motor deficits and α-syn pathology in Lrrk2 R1628P mice. Our findings elaborate on the mechanism that E. coli triggers α-syn pathology in Lrrk2 R1628P mice, and highlight a novel gene-environment interaction pattern in LRRK2 risk variants. Even more importantly, the findings reveal the interplay between the specific risk gene and the matched environmental factors triggers the initiation of α-syn pathology in sPD."
So eating a lot of PUFA from seed oil gives you not only a risk of IBD, but also Parkinson's.
Here is a study of another problem with PUFA. We are constantly producing ROS in the mitochondria, and we know from animals that have a lot of PUFA near there mitochondria, they don't live as long as animals that favor more saturated fats near there mitochrondia. This is a study that Ray Peat mentioned in his last newsletter:
https://sci-hub.se/10.1016/j.bbabio.2006.01.009
"ROS can damage many different kinds of cellular macromolecules including lipids, proteins and DNA. Damage to DNA
may be the most important for aging because it can lead to
irreversible loss or alteration of genetic information in postmitotic cells. mtDNA is situated very close to or even in
contact with the site of mitochondrial ROS production. Since
long-lived vertebrates have low rates of MitROS generation,
this should affect the level of oxidative damage and somatic
mutations in their mtDNA. In agreement with this notion it has
been found that brain and heart 8-oxodG in mtDNA correlates
negatively with maximum longevity in mammals and birds
[39]. This agrees with the lower urinary excretion of 8-oxo-7,8-
dihydroguanine of long-lived animals [70]. In addition, the
levels of 8-oxodG were around 10 fold higher in mtDNA than in
nDNA in the brain and heart of all the 11 studied mammalian
and bird species studied [39,71], a difference similar to that
observed for spontaneous mutations comparing both DNAs.
That suggests that the flux rates of both ROS attack on and
repair of DNA are much higher in the mtDNA of short-lived
than long-lived animals, and are also much higher in the
mtDNA than in the nDNA of all species irrespective of their
longevity [33]. The higher rate of MitROS production of shortlived animals may be an important cause of their much faster
rate of accumulation of mtDNA mutations during aging. A
similar degree of accumulation of mtDNA mutations occurs
after 70–100 years in humans, after 35–50 years in chimpanzees [72] and after only 2–3 years in mice [73].
Unsaturated fatty acids of cellular membranes are the
macromolecules most susceptible to oxidative damage in
cells, and this sensitivity increases as a function of their number
of double bonds. We have found that the cellular membranes of
long-lived mammals and birds have low degrees of fatty acid
unsaturation in mitochondria and tissues including liver, heart,
skeletal muscle, and kidney, and this constitutively protects
their cellular membranes, proteins and DNA against lipid
peroxidation-derived damage [74–77]; reviewed in [78,79].
This is shown in Fig. 1A for heart phospholipid fatty acids in the
heart of 8 animal species with different MLSP [76]. The total
number of double bonds (DBI = double bond index) was
negatively correlated with maximum longevity (Fig. 1A) and
the same was true for the sensitivity to lipid peroxidation (not
shown). Similar results were obtained in liver tissue [77] and
liver mitochondria and their phospholipid classes [75,80] in
different mammalian species, as well as in birds (longer-lived)
compared to mammals of similarly body size. Long-lived
animals obtain a low DBI mainly by avoiding highly
unsaturated fatty acids like 22:6n-3, and sometimes 20:4n-6,
substituting them mainly for 18:3n-3 and 18:2n-6. This lowers
their degree of unsaturation without changing the total amount
of polyunsaturated fatty acids, allowing a strong decrease in
sensitivity to lipid peroxidation probably without major changes
in membrane fluidity, a “homeoviscous-longevity adaptation”
[78]. On the other hand, lipid peroxidation generates aldehydic
products, like malondialdehyde (MDA) and others, that
covalently attach to protein lysine residues. Recently we
found that the level of MDAL protein adducts negatively
correlates with maximum longevity in the heart of different
mammalian species (Fig. 1B) [81]. Thus, the longer the life span
of a species, the lower is its fatty acid double bond content, its
sensitivity to lipid peroxidation and its level of lipoxidationderived protein modification. Bird (long-lived) species also
show lower fatty acid unsaturation and sensitivity to lipid
peroxidation in liver and heart mitochondria (reviewed in [78]),
lower levels of aminoadipic and glutamic semialdehydes
(specific protein carbonyls) and lower levels of CML, CEL
and MDAL in brain proteins than the corresponding comparable
mammals [82]. The relationship between fatty acid unsaturation
and oxidative damage is also observed in experimental studies in
vivo. We have recently observed that treating rats with dietary
oils with a low number of double bonds lowers the degree of
fatty acid unsaturation of brain cellular membranes and lowers
brain lipoxidation-derived protein modification and 8-oxodG
levels in brain mtDNA [83]. This makes sense because lowering
fatty acid unsaturation decreases the susceptibility of membranes to lipid peroxidation. Lipid peroxidation-derived endproducts (“enals”) can also react at the exocyclic amino groups
of dG, dA, and dC to form various alkylated products[84]. Some
common enals that cause DNA damage, analogously to proteins,
are MDA, acrolein, and 4-hydroxynonenal, among others.
Common adducts arising from enals are exocyclic adducts such as etheno adducts, and M1dG. These DNA damage markers are
mutagenic, carcinogenic, and have powerful effects on signal
transduction pathways. Furthermore, they (a) are present in the
genome of healthy humans and other animal species; (b) are
efficient premutagenic lesions that induce mutations frequently
detected in oncogenes or tumor suppressor genes from human
tumors; (c) show increased levels in aged animals; and (d)
!!increase nearly 20 fold with a high PUFA diet!!. Thus, lipid
peroxidation may be a significant endogenous source of DNA
damage and mutations." -
Thanks for sharing your thoughts. From what I gather, you seem to agree with me on healthy user bias being the main reason for the association.
"The healthy user effect is best described as the propensity for patients who receive one preventive therapy to also seek other preventive services or partake in other healthy behaviors.18 Patients who choose to receive preventive therapy may exercise more, eat a healthier diet, wear a seatbelt when they drive, and avoid tobacco. As a result, an observational study evaluating the effect of a preventive therapy (e.g., statin therapy) on a related outcome (e.g., myocardial infarction) without adjusting for other related preventive behaviors (e.g., healthy diet or exercise) will tend to overstate the effect of the preventive therapy under study. The healthy user effect has been widely cited as a likely source of bias in observational studies of HRT. Studies indicate that women who took HRT were more likely to engage in healthy behaviors such as regular exercise, a healthy diet, abstinence from alcohol, and maintenance of a healthy weight as compared to non-users.2 The apparent protective effect of HRT on cardiovascular disease likely reflects these unmeasured differences in patient characteristics."
In this case, the "preventive therapy" would be eating more PUFAs.
Underreporting alcohol and energy intake could be thought of as an extension of healthy (or in this case unhealthy) user bias
-
Based on the two studies you posted that I don't consider "real life", they analyze fat consumption and the occurrence of diseases and draw a conclusion, with absolutely no information other than the type of fat (one of them is based on a questionnaire that the person has to answer, it's not even a follow-up). Did they have any nutritional deficiencies? What was their calorie intake like? Did they exercise? What kind of exercise? Did they sunbathe? How was their social life like? Was work stressful? After that you have studies linking the consumption of PUFAs to a reduction in some marker that they say causes/increases such a disease, like cholesterol, and based on this isolated marker they conclude that PUFA is good, you see this quite often when it comes to omega 6, that's why there's this emphasis on the balance between omega 3 and omega 6 because then the problem isn't omega 6 but the omega3:omega6 ratio...
It's very difficult to have a human study comparing a deficiency of essential fatty acids with a replete of essential fatty acids. The "essential" status makes it unethical to carry out such an experiment on humans, which is another reason why most of them are based on rats, even in super-artificial environments, and in these cases the indication of the relationship between PUFAs and inflammation becomes clearer because you have studies of the resistance of these "EFA-deficient" mice that are practically immune to autoimmune diseases such as type 1 diabetes, glomerulonephritis, resistant to inflammation, endotoxin, etc. ..
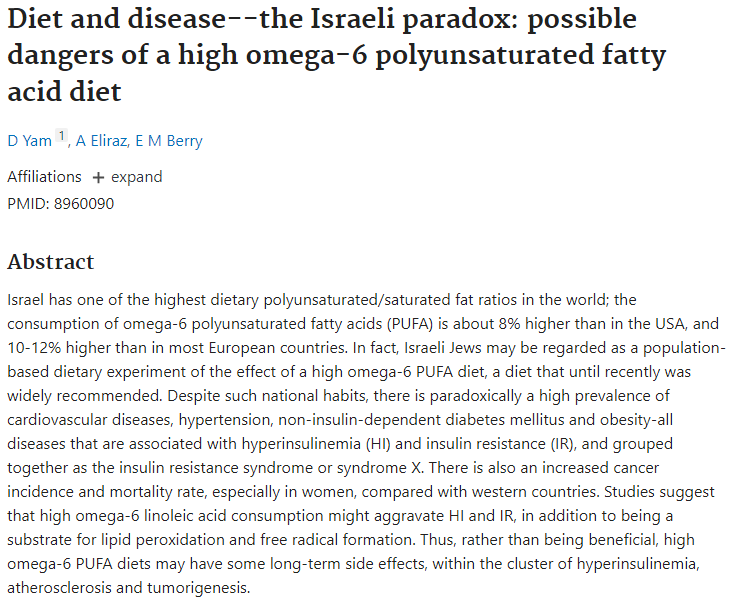
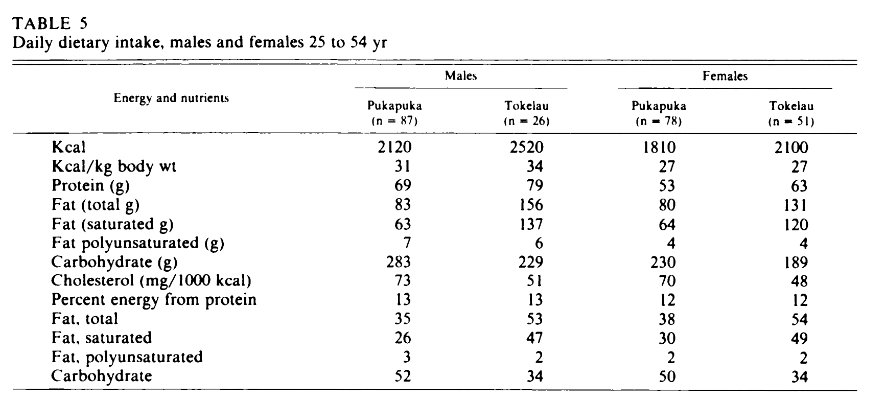
In "real life" we can only look for very detailed studies or examples (such as Israel and its high consumption of PUFAs vs. Okinawa before 2000s consuming 4.8g PUFA/day, or Japan consuming around 6g PUFA/day, Tokelau before seed oils/PUFA).
But that's my opinion, of course.
-
https://www.bmj.com/content/346/bmj.e8707
https://www.bmj.com/content/353/bmj.i1246
https://pubmed.ncbi.nlm.nih.gov/4100347/
https://www.sciencedaily.com/releases/2020/01/200117080827.htm
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2640413/
https://lipidworld.biomedcentral.com/articles/10.1186/s12944-020-01256-0
https://pubmed.ncbi.nlm.nih.gov/21256145/
https://www.sciencedaily.com/releases/2017/12/171207141624.htm
https://pubmed.ncbi.nlm.nih.gov/18710653/?dopt=AbstractPlus
https://pubmed.ncbi.nlm.nih.gov/20172549/?dopt=AbstractPlus
https://pubmed.ncbi.nlm.nih.gov/18029129/
https://pubmed.ncbi.nlm.nih.gov/12398924/
https://pubmed.ncbi.nlm.nih.gov/8640909/
https://pubmed.ncbi.nlm.nih.gov/17656037/
-
Researchers obviously control for relevant variables such as energy intake, socioeconomic status etc. What reason is there to believe work stress or social life would significantly differ between thosa at low vs high PUFA intake?
I agree that looking at biomarkers such as cholesterol is not a reliable way of assessing a persons health. But studies looking at hard outcomes paint the same picture in favor of PUFA.
Ray Peat was against both omega 3 and 6...
-
Are high omega-6 seed oil good?
Even Chat GPT considers MUFA-rich fats better for cooking than omega-6 rich fats such as soy oil or sunflower oil. I think the recent scientific consensus is not in favor of high PUFA seed oils, at least not according to Chat GPT.Omega-3/omega-6 balance
The reason they point out is that omega-6 should be balanced out with omega-3. I think this is a valid concern TBH. Ray Peat never admitted that. But I think he never found out the problems of too much omega-6, as he always drank milk, containing omega-3.My girlfriend and I eat basically the same diet. Except that I eat diary and she can not tolerate it. She will get eczema from too much chicken, while I won't. If she supplements krill oil the eczema goes away.
So how much total PUFA is best?
Now if you avoid high omega-6 food, you need very little total PUFA too balance it out. Dairy/beef/lamb are already in perfect balance. So even according to mainstream science, you won't need to supplement fish oil or whatever.I talked a bit with Chat GPT and he buys parts of the Ray Peat theory that high PUFA might decrease lifespan:
"Omega-3 fatty acids, found abundantly in fish, are polyunsaturated, meaning they contain multiple double bonds in their chemical structure. This makes them more susceptible to oxidation, a process that can produce reactive oxygen species (ROS) and lead to oxidative stress within cells, including damage to mitochondrial DNA (mtDNA). There's a hypothesis suggesting that species with a higher proportion of saturated fats (which have no double bonds) in their cell membranes may experience less oxidative damage, potentially contributing to increased longevity.
The concern is that a high intake of polyunsaturated fats (PUFAs), by increasing the double bond index, could theoretically increase susceptibility to oxidative damage, affecting cellular aging and potentially impacting longevity across species. This is because PUFAs, including those from omega-3 rich fish, when oxidized, can harm cellular components, including mtDNA.
Despite the theoretical concerns about oxidative stress and longevity, omega-3 fatty acids from fish are well-documented to offer significant health benefits. These include reducing the risk of heart disease, supporting brain health, and providing anti-inflammatory effects. These benefits are largely attributed to their ability to improve lipid profiles, decrease blood pressure, and modulate inflammatory responses.
A key aspect of consuming omega-3 rich foods like fish is to balance the dietary intake of omega-6 and omega-3 fatty acids. Many diets are disproportionately high in omega-6 fatty acids, which can promote inflammation when not balanced by adequate omega-3 intake. Consuming fish 2-3 times a week can help achieve a healthier omega-6/omega-3 ratio, reducing the risk of chronic diseases and supporting overall health.
While omega-3 fatty acids are essential and beneficial, the principle of moderation applies. Consuming fish within recommended amounts (2-3 times a week) is advised to garner the health benefits without the potential risks associated with high levels of PUFAs. This approach ensures adequate intake of omega-3s to balance out omega-6 fatty acids, without necessarily exceeding what is needed for health benefits."
So if too much PUFA is bad, should we eat MUFA or SFA?"
So I think the mainstream science converged slowly to,
"Don't eat too much PUFA seed oils, but use MUFA (olive oil) instead."
Milk is quite high in MUFA as well. And Ray Peat said in some interviews that the main fats in your diet should be some balance between stearic acid, palmitic acid and oleic acid.Personally, I think MUFA can be in some cases more beneficial for treating acute inflammation problems than SFA. But SFA boosts your sex hormones much more. I can imagine that some studies found that health improves by avoiding SFA, but keeping avoiding it will make sure you never reach the next level of health IMO, which is low inflammation + awesome hormones.
-
You'd be surprised by the lack of control in studies, sometimes of variables that have a major influence.
"What reason is there to believe work stress or social life would significantly differ between thosa at low vs high PUFA intake?"
The problem is not believing that it differs, the problem is that a study that seeks to elucidate the susceptibility of a group to diseases that only looks at the type of fat is a joke lol. Since one of the biggest contributors to disease and inflammation is chronic stress, and you're analyzing the susceptibility of certain groups to disease, it's a pretty important reason to consider.
There is no "Japan Paradox" due to low consumption of PUFA(at least in the past), there is no "Tokelaun paradox" due to the very high consumption of saturated fat in the past, but there is an "Israeli paradox" and their high consumption of vegetable oils and high incidence of diseases.
"Vascular disease is uncommon in both populations and there is no evidence of the high saturated fat intake having a harmful effect in these populations."
-
@Kasper
Is there a reason to believe stress levels would be higher among people consuming less PUFAs? Because that's what you're implying here.If you have a large enough sample, there's no reason to assume stress levels would be significantly different between those at low vs high intakes of PUFA, thus it's pointless to account for chronic stress in such an analysis. The point of these studies is precisely to isolate the effect of PUFA specifically on health outcomes.
Ecological studies like the Israeli or Japanese ones are arguably far more confounded and less relevant than the meta analysis I posted. Is it the lack of PUFA that made Tokelauans healthy or the myriad of other factors that distinguishes them from the average westerner?