Low salt diet and water restriction
-
@NNight I was on such a diet and lost a lot of weight, but I had constant weakness and when I got out of bed or from a chair, my eyes grew dark (possibly due to decreased blood pressure)
-
@alex155 thanks for describing what you experienced!
I tend to be on the higher side of blood pressure (before trying, and I don't measure it often), so that might be a good news.
It's possible that it should remain a short term diet (@heteronormie
 ).
). -
Copy-paste of a post I've written elsewhere.
This is about dry fasting but it remains interesting in this context:Cancer cells have multiple hallmarks and two of them are that (1) they don't burn glucose efficiently (this is called the Warburg effect) and (2) they contain too much water. By the way, genetic mutations found in cancer cells are also thought (not by the mainstream view) to be the consequence of the metabolic issues instead of a cause of cancer.
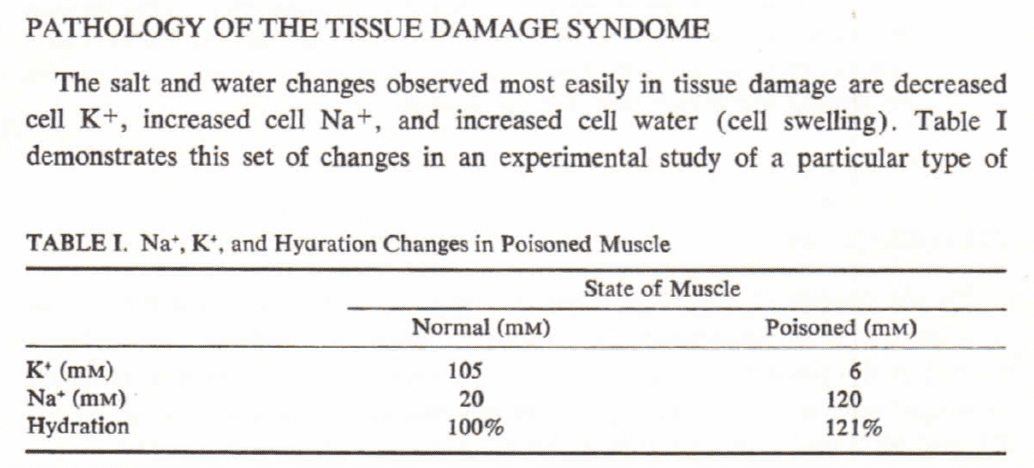
The Warburg effect is thought by some scientists to be due to the fact that oxygen has trouble reaching mitochondria, the site of glucose metabolism, so that "oxidative phosphorylation" (which is the name of the proper metabolism of glucose, involving oxygen) is not possible. Their explanation is that the Warburg effect is linked to the water excess. Here is an excerpt of a publication explaining this:
More than 80 years ago Nobel Prize laureate Warburg pointed out that in cancerous cell the loss of oxidative capacity of mitochondria and the glycolytic metabolism shift relative to oxidative phosphorylation as O2 could not reach to mitochondria. However, the nature of the primary mechanism leading to generation of Warburg phenomenon has not been elucidated yet.
In 1971 the second revolutionary discovery was made in cancer research by Raymond Damadian, who elucidated that cancerous cell is markedly overhydrated and can be much as 90% water while in norm it can be 70-73%. “Magnetic Resonance” method [2] of detection of cell over hydration suggested by him which serves as an early tumor detection diagnostic method at present has a worldwide clinical usage.
It is established that cell swelling triggers its proliferation, while cell shrinkage promotes its apoptosis [3-6]. Cell hydration causes not only the promotion of cell division and oncogene expression but also inactivates genes inducing cell apoptosis [7]. On the basis of these data cell over hydration was suggested as a primary messenger in carcinogenesis [3,7]. However, the nature of metabolic mechanism the dysfunction of which causes over hydration in cancer cells as well as the link between cell over hydration and Warburg phenomenon are also not elucidated yet. Therefore, it is suggested that the discovery of intracellular signaling pathway through which the correlation between cell hydration and mitochondrial function is realized could be one of the key problems of modern cancer research. [...]
As CO2 solubility in aqua medium is more than 20 times higher than O2 solubility [28], oxygen could not reach to mitochondria and would lead to generation of Warburg phenomenon. Therefore, prevention of generation of Warburg phenomenon can be achieved by both cell dehydration and the decrease of CO2 solubility in cytoplasm.Moreover, dry fasting might help with the release of the water excess (edema), as hypothesized in the following publication:
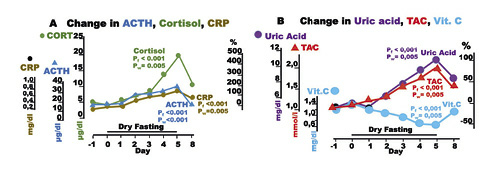
Despite the absolute Na+, K+, and water deprivation and the respective adjustments through Days 1–5, participants continued to excrete significant amounts of all three substances. Under this consideration, DF had natriuretic, diuretic, and kaliuretic effects. The natriuretic and diuretic effects contribute significantly to edema elimination. [...]
The association of adrenaline and EPO with both edema elimination (Fig. 2) and improved cellular oxygenation raises the question of whether edema elimination and improved cellular oxygenation are causally linked. This question is apparently of paramount therapeutic importance.Dry Fasting Physiology: Responses to Hypovolemia and Hypertonicity
-
Also, vasopressin (antidiuretic hormone) might be helpful because it could shuttle potassium in the cells:
Within the 24 hour period after ADH injection, about 300~Eq of potassium were retained by each animal. Since serum potassium concentration did not change significantly, the bulk of retained potassium must have entered compartments other than the extracellular space. Since total renal potassium content in male Wistar rats of comparable body weight is about 120~Eq (unpublished observation), any increase in renal potassium content would contribute only slightly to the compartmentalization of the retained potassium. Therefore, the bulk of the retained potassium must have entered cells of extrarenal tissues. However, this argumentation demands further experimental proof.
ADH-induced potassium retention in rats with genetic diabetes insipidus
Could the consumption of high potassium foods, low salt and low water (increased antidiuretic hormone but without too much water retention) be a good way to improve cellular health?
-
The connections between water homeostasis, hyperosmolarity and the thyroid system are listed below:
- There exist theoretical arguments allowing us to hypothesize that hyperosmolarity, induced by water restriction for example, could facilitate the synthesis of thyroid hormones while potentially lowering the requirement for TSH stimulation.
- Rats (with an animal model of hypothyroidism) put under water restriction got an increase in their T3 levels, bringing them almost back to the control group’s levels.
- It was found that, in rabbits, vasopressin itself seems to play a role similar to TSH regarding thyroid hormone synthesis.
- Two studies on rats found that water restriction or deuterium depleted water (which might be interpreted by the body as water restriction) tend to lower TSH levels.
- Finally, bile acids could be related both to the TSH and metabolic rate of tissues involved in thermogenesis, but are also related to water homeostasis as the bile acid TGR5 receptor (along with the FXR transcription factor) is involved in kidneys’ function. From this data, we can hypothesize that a TSH decrease itself could boost T3 systemic levels as it might increase bile acids synthesis and thus peripheral deiodinase enzymes.
Thus, water restriction (or deuterium depletion) could lead to a TSH decrease while keeping thyroid hormones levels maintained or increased. The TSH decrease could be explained by an increase in vasopressin, which could play the role of a TSH surrogate and stimulate bile acids synthesis and thus the conversion of T4 to T3 in peripheral tissues.
Another explanation could be that hyperosmolarity itself, by activating the NFAT5 transcription factor which would upregulate the uptake of inositol by the thyroid, or activating the CREB3L1 transcription factor, would increase the sensitivity of the thyroid gland to TSH and optimize thyroid hormones output.
Upping intake of inositol, selenium and intermittently restricting water intake to achieve hyperosmolarity may improve the function of the thyroid system. -
@NNight said in Low salt diet and water restriction:
By the way, genetic mutations found in cancer cells are also thought (not by the mainstream view) to be the consequence of the metabolic issues instead of a cause of cancer.
Oh by the way

Amazing info drops in this thread
 (don't miss that substack).
(don't miss that substack). -
@ThinPicking thanks, that's kind of you

-
The decrease in the cytoplasmic kosmotropic osmolytes gradually transforms the structured water into unstructured water, which eventually causes a reduction in the order-information degree of the cellular thermodynamic-energy system, which upon reaching the maximum tolerable entropy, causes the cell a “near-death state”.
Measures that transform unstructured water into structured water, such as peritumoral hyperosmolality and increased intracellular kosmotropic osmolytes, and strategies that increase mitochondrial oxidative phosphorylation may restore physiological and cellular bioenergetics. The restoration of these metabolic parameters will provide the necessary information to reestablish order, organization, and compartmentalization that can stop neoplastic cells proliferation, promote differentiation, and restore cellular metabolic harmony.
Research efforts have suggested that the promotion of hyperosmolarity can be used as a form of treatment. Hyperosmolarity increases EZ water inside the cell, which in turn promotes apoptosis. This approach has a minimal effect on neighboring healthy cells, suggesting this treatment as a possible option for cancer. This treatment would function by restoring the structured water with the appropriate levels of EZ zones back into the cell. By doing so, the cell returns to its normal state of order and organization, which enables the cell to continue its normal metabolic course which includes reestablishing apoptosis.
Structured Water and Cancer: Orthomolecular Hydration Therapy
-
Low salt raises aldosterone and I think prolactin too. Aldosterone helps you retain sodium by disposing potassium and magnesium, I don't think you want that.
-
-
@izkrov said in Low salt diet and water restriction:
Low salt raises aldosterone and I think prolactin too. Aldosterone helps you retain sodium by disposing potassium and magnesium, I don't think you want that.
In a kidney cell:
MR expression is tightly regulated by osmotic stress. Hypertonic conditions induce expression of tonicity-responsive enhancer binding protein, an osmoregulatory transcription factor capable of binding tonicity-responsive enhancer response elements located in MR regulatory sequences. Surprisingly, hypertonicity leads to a severe reduction in MR transcript and protein levels. [...] In sharp contrast, hypotonicity causes a strong increase in MR transcript and protein levels.
-
@NNight I don't really understand what MR gene expression is. Could you explain?
-
Aldosterone effects are mediated by the mineralocorticoid receptor (MR), a transcription factor highly expressed in the distal nephron. Given that MR expression level constitutes a key element controlling hormone responsiveness, there is much interest in elucidating the molecular mechanisms governing MR expression.
This means that the mineralocorticoid receptor (which mediates the effects of aldosterone) expression might be reduced in conditions of water restriction ("osmotic stress").
Thus, you might (this is an in vitro study) want to restrict water consumption when you limit your salt intake, and vice versa.
-
My latest fad is molybdenum (that's not my first time).
It could be helpful to increase uric acid which seems to be needed during "dehydration" (or dry fasting at least):
Also, it is thought to be able to chelate unbound copper while copper could be impairing transcription factors:
Nevertheless, what is the link between a selective LXR activation and copper homeostasis?
First, copper may bind with high affinity to the DNA‐binding domain of several nuclear receptors, including LXRs, inducing a conformational change that prevents DNA binding and, in turn, their transcriptional activity.
Liver X receptors and copper metabolism: New frontiers for the oxysterol receptorsPs:
Another theory, first proposed in the 1950s, suggests that uric acid is structural homolog of caffeine (which in turn is a structural homolog of adenosine), and that high uric acid levels promoted mental alertness for primates and contributed to the development of human intelligence [8]. This hypothesis has been increasingly supported by experimental observations, although its role in evolution remains to be confirmed.
-
Caffeine inhibits hypothalamic A1R to excite oxytocin neuron and ameliorate dietary obesity in mice
We also show that caffeine excites oxytocin expressing neurons, and blockade of the action of oxytocin significantly attenuates the effect of caffeine on energy balance.
Was Ray Peat "against" oxytocin?
-
@NNight said in Low salt diet and water restriction:
Caffeine inhibits hypothalamic A1R to excite oxytocin neuron and ameliorate dietary obesity in mice
Was Ray Peat "against" oxytocin?
I thought this was an interesting question.
User: was ray Peat against oxytocin
Peatbot: I don't know.
My second attempt at finding an answer:
User: is oxytocin healthy?
Peatbot: Oxytocin is a hormone that plays various roles in the body, including in social bonding, sexual reproduction, childbirth, and the period after childbirth. It is often referred to as the "love hormone" or "cuddle hormone" because it is released when people snuggle up or bond socially. However, its effects are not universally positive.
According to the context provided, oxytocin is described as one of the adaptive hormones that can have stress-related responses. It is not solely a "happiness and euphoria hormone" because it can also increase under stress, and its effects are not always beneficial. This suggests that while oxytocin has important functions, it is not inherently "healthy" or "unhealthy" but rather has complex roles that can vary depending on the situation.
I hope this helps.
-
@NNight Inosine could also help with the uric acid. During a low water diet, I feel thirst decreased when taking that.
-
@Razvan
Also adding P5P and zinc to this low water intake cleared more weight out. Lost much more weight overnight, prolactin? -
@DavidPS thanks!
This Peatbot is quite good for an AI.
That's the impression I've got from reading articles about oxytocin too (and what I've read from Haidut was less "balanced" than these conclusions, but he can have differing opinions from Ray Peat). However, the interpretation of oxytocin effects might be "biased" by how research is done, e.g. supplementing oxytocin with a nasal spray, when oxytocin levels are associated with vasopressin levels, potential other hormones (like secretin) or physiological parameters, and "side effects" could happen if you "de-correlate" them (for example hypo-osmolarity).@Razvan
Interesting, I've never tried inosine nor P5P.
Last time I took zinc, I had a very strong metallic/strange taste (it was a sort of colloidal solution) and had to spit it out. Made me wondered if I had too much zinc (while I was not even supplementing chronically at the time). -
Could oxytocin be helpful as it can bind free copper ions in the cells?
Copper and silver ions seem to impair LXR and FXR activation. This is not necessarily a good thing and could be a cause of symptoms seen in copper overload situations (e.g. Wilson's disease):
Together, these data demonstrate that copper-mediated nuclear receptor dysfunction disrupts liver function in WD and potentially in other disorders associated with increased hepatic copper levels.
Elevated copper impairs hepatic nuclear receptor function in Wilson’s diseaseIs this still true when copper is bound to oxytocin?
In this work, we focus on characterizing copper and zinc bound forms of oxytocin and related analogs through far-UV circular dichroism. We report that Cu(II) and Zn(II) bind uniquely to oxytocin and all analogs investigated. Furthermore, we investigate how these metal bound forms may affect downstream signaling of MAPK activation upon receptor binding. We find that both Cu(II) and Zn(II) bound oxytocin attenuates the activation of the MAPK pathway upon receptor binding relative to oxytocin alone.
Metal-induced structural changes to a peptide hormone may have a number of effects on storage, secretion, stability, and/or signaling. In this case, it is possible that both Zn(II) and Cu(II) lend different structural integrities to oxOT at different points in oxOT lifetime. Physiologically, it is possible that Cu(II) is bound to oxOT in serum but, because the concentrations of metal ions surrounding specific tissues are believed to fluctuate, Zn(II) may be able to displace Cu(II) under specific concentrations. It still remains to be seen how Cu(II) would affect oxOT in serum, however, metal binding may be a key player in prevention of degradation; further studies in our lab are underway to test this hypothesis. The binding of metal ions to peptide hormones, particularly oxOT, may provide an additional source for regulation, and this study provides the foundation for future studies.
Investigation of metal modulation of oxytocin structure receptor-mediated signaling
It would be interesting to determine if such an effect (oxytocin binding to copper thus avoiding free copper to disturb FXR and LXR, or other nuclear receptors, activation) could be "significant" in terms of the number of moles of oxytocin with respect to the quantity of copper ions in a cell.