High-starchy carbohydrate diet aggravates NAFLD by increasing fatty acids influx mediated by NOX2
-
Abstract
Nonalcoholic fatty liver disease (NAFLD) is a high-incidence lipid disorder that affects more than a quarter of the population worldwide, and dietary intervention is the recognized treatment. Starch is the main component of staple foods that are consumed daily, and the effects, metabolic pathway, and molecular mechanism of starch in the context of NAFLD remain unclear. Our study showed that a high-starch carbohydrate diet (HCD) led to the occurrence and exacerbation of NAFLD in mice. Transcriptomics and metabonomic analyses showed that the increased fatty acid influx mediated by NADPH oxidase 2 (NOX2) exacerbated NAFLD. Knocking down NOX2 specifically alleviated HCD-induced NAFLD in vivo and in vitro. Moreover, the large amounts of ROS produced by NOX2 further exacerbated insulin resistance and increased lipolysis in perirenal white adipose tissue (periWAT), thereby providing fatty acids for hepatic lipid synthesis. In addition, the interaction between AMPKα1 and p47phox was the pathway that mediated the high expression of NOX2 induced by a HCD. Our study systematically demonstrated the effect of a HCD on NAFLD. Elevated fatty acid influx is a unique molecular regulatory pathway that mediates HCD-induced NAFLD exacerbation, which is different from the effect of simple sugars. Additionally, NOX2 was suggested to be a specific and effective drug target for NAFLD.
https://www.sciencedirect.com/science/article/pii/S2213453022002452 -
Dairy product consumption was associated with a lower likelihood of non-alcoholic fatty liver disease: A systematic review and meta-analysis
Abstract
Background and aims
Non-alcoholic fatty liver disease (NAFLD) is one of the most common causes of chronic liver disease. Several epidemiological studies attempted to assess the association between dairy product and the likelihood of NAFLD, but the contribution of dairy consumption to NAFLD remains controversial. We conducted a meta-analysis to investigate the association between dairy product consumption and NAFLD.Methods
We conducted a literature search using the PubMed, Web of Science and Scopus databases, we conducted a thorough search of the literature published before January 5, 2023. Combined odds ratios (ORs) and 95% confidence intervals (CIs) of NAFLD in relation to dairy product intake were estimated using random-effects models. Subgroup analysis and meta-regression were performed according to the study design, region, sex, body mass index (BMI), type of exposure, NAFLD diagnostic criteria, and exposure assessment tools.Results
We initially identified 4,634 relevant studies, of which 25 complied with the inclusion criteria, including seven cross-sectional studies, six case–control studies and one cohort study. A total of 51,476 participants (14,546 patients with NAFLD) were included in the meta-analysis. There was an inverse association between dairy product consumption and NAFLD (OR = 0.97, 95% CI = 0.94–0.99). Subgroup analysis demonstrated that lower likelihood of NAFLD was associated with dairy product consumption in subgroups of Asian populations, women, patients diagnosed using NAFLD-related scores, patients with a BMI of 18.5–24.9 kg/m2, dairy intake assessed using a food frequency questionnaire, milk consumption, and yogurt consumption. No noteworthy connection was observed in the other subgroups.Conclusion
Our meta-analysis findings revealed that dairy product consumption is inversely associated with NAFLD. Consumption of dairy products could help prevent the development of non-alcoholic fatty liver disease.Keywords: milk, non-alcoholic fatty liver disease, dairy, meta-analysis, systematic review
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9992538/ -
That's remarkable. Especially since the high fat diet contained twice the amount of soybean oil compared to the high starch diet.
It seems that (at least in this animal study) that high starch is worse than high PUFA, which I didn't expect.
It might have gone differently with potatoes starch or well cooked starch.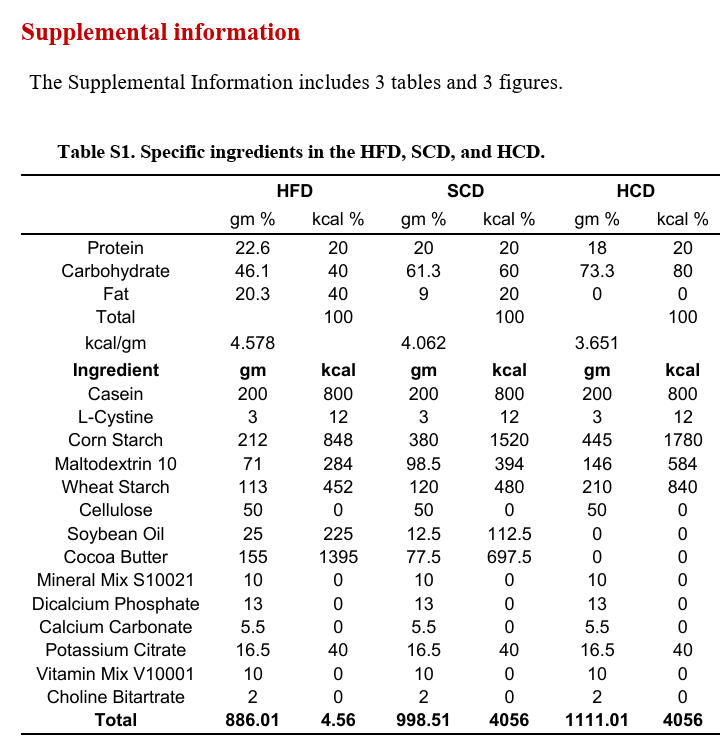
-
@Mauritio is there markers for undercooked vs well cooked starch? Like anything quantitative or just use time under heat as metric?
-
@Mauritio said in High-starchy carbohydrate diet aggravates NAFLD by increasing fatty acids influx mediated by NOX2:
It might have gone differently with potatoes starch or well cooked starch.
I agree but would I would have stated it more firmly.
User: does persorption effect the liver
Peatbot.com: Yes, persorption can affect the liver. Gerhard Volkheimer's research found that starch grains, when ingested, could be found in various bodily fluids, including the blood. These starch grains can block arterioles in different organs, including the liver, leading to the death of cells that depend on the blood supplied by those arterioles. This blockage and subsequent cell death can impair the liver's functions. Additionally, the presence of foreign particles like starch grains in the liver can have immunological implications and contribute to liver diseases.
-
@thyroidchor27 I just use time and how my body reacts to it as a measure
-
Inverse Association of Fruit and Vegetable Consumption with Nonalcoholic Fatty Liver Disease in Chinese Patients with Type 2 Diabetes Mellitus
Abstract
We aimed to investigate the association of fruit and vegetable consumption with nonalcoholic fatty liver disease (NAFLD) in Chinese patients with type 2 diabetes mellitus (T2DM). This cross-sectional study included 2667 Chinese patients with T2DM aged 18 to 76 years from March 2017 to October 2021. Dietary intake was assessed using a food frequency questionnaire, and prevalent NAFLD was diagnosed with abdominal ultrasonography. High fruit–vegetable consumption was determined using ≥500 g/day consumption of both fruit and vegetable, and both fruit and vegetable consumption were divided into three categories of <200 g/day (low), 200–400 g/day (median) and >400 g (high). The primary outcome measurement was multivariate-adjusted odds ratios (ORs) with 95% confidence intervals (CIs) for the prevalence of NAFLD in relation to the highest fruit and (or) vegetable intake compared with the lowest. Secondary analyses were conducted to assess the effects of either fruit or vegetable intake on the fatty liver index (FLI) using multivariable linear regressions. There were 1694 men and 973 women in this study, and 1445 (54.06%) participants had prevalent NAFLD. Patients with high fruit–vegetable intake had a lower prevalence of NAFLD than those with low fruit–vegetable intake (52.04% vs. 56.48%), but this difference was not statistically significant (p = 0.065). Vegetable intake had a significantly inverse association with NAFLD (OR: 0.68, 95% CI: 0.52–0.90), but this association was not pronounced with fruit intake (OR: 1.23, 95% CI: 0.89–1.69) or fruit–vegetable intake (OR: 0.90, 95% CI: 0.73–1.10). Additional analyses showed that an increase in vegetable intake was linearly associated with a significant reduction in FLI (β: −1.028, 95% CI: −1.836, −0.219). In conclusion, higher vegetable consumption was associated with lower odds of NAFLD in Chinese patients with T2DM, which suggested that increased vegetable intake might protect patients with diabetes against NAFLD.
Keywords: NAFLD; dietary; type 2 diabetes mellitus; fruit and vegetable
https://www.mdpi.com/2072-6643/14/21/4559 -
Fructose and Sugar: A Major Mediator of Nonalcoholic Fatty Liver Disease
Nonalcoholic Fatty Liver Disease (NAFLD) is the hepatic manifestation of metabolic syndrome, and its rising prevalence parallels the rise in obesity and diabetes. Historically thought to result from overnutrition and sedentary lifestyle, recent evidence suggests that diets high in sugar (from sucrose and/or high fructose corn syrup (HFCS)) not only increases the risk for NAFLD, but also, nonalcoholic steatohepatitis (NASH). Here we review the experimental and clinical evidence that fructose precipitates fat accumulation in the liver, due to both increased lipogenesis and impaired fat oxidation. Recent evidence suggests that the predisposition to fatty liver is linked with metabolism of fructose by fructokinase C, resulting in ATP consumption, nucleotide turnover and uric acid generation that mediate fat accumulation. Alterations in gut permeability, microbiome, and associated endotoxemia contributes to the risk of NAFLD and NASH. Early clinical studies suggest that reducing sugary beverages and total fructose intake, especially from added sugars, may have a significant benefit on reducing hepatic fat accumulation. We suggest larger, more definitive trials to determine if lowering sugar/HFCS intake, and/or blocking uric acid generation, may help reduce NAFLD and its downstream complications of cirrhosis and chronic liver disease.
Keywords: hepatic steatosis, hepatic inflammation, insulin resistance, sugar consumption, uric acid
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5893377/ -
Brown Rice Inhibits Development of Nonalcoholic Fatty Liver Disease in Obese Zucker (fa/fa) Rats by Increasing Lipid Oxidation Via Activation of Retinoic Acid Synthesis
Abstract
Background
White rice and its unrefined form, brown rice, contain numerous compounds that are beneficial to human health. However, the starch content of rice can contribute to obesity, a main risk factor for nonalcoholic fatty liver disease (NAFLD).Objectives
We investigated the effect of rice consumption on NAFLD and its underlying molecular mechanism.Methods
We randomly divided 7-week-old male obese Zucker (fa/fa) rats, an animal model of NAFLD, into 3 groups (n = 10 each) fed 1 of 3 diets for 10 weeks: a control diet (Cont; AIN-93G diet; 53% cornstarch), a white rice diet (WR; AIN-93G diet with cornstarch replaced with white rice powder), or a brown rice diet (BR; AIN-93G diet with cornstarch replaced with brown rice powder). Liver fat accumulation and gene expression related to lipid and vitamin A metabolisms, including retinoic acid (RA) signaling, were analyzed.Results
Hepatic lipid values were significantly decreased in the BR group compared with the Cont group, by 0.4-fold (P < 0.05). The expression of genes related to hepatic fatty acid oxidation, such as carnitine palmitoyltransferase 2, was approximately 2.1-fold higher in the BR group than the Cont group (P < 0.05). The expression of peroxisomal acyl-coenzyme A oxidase 1 and acyl-CoA dehydrogenase medium chain was also significantly increased, by 1.6-fold, in the BR group compared with the Cont group (P < 0.05). The expression of VLDL-secretion-related genes, such as microsomal triglyceride transfer protein, was also significantly higher in the BR group (2.4-fold; P < 0.05). Furthermore, aldehyde dehydrogenase 1 family member A1, an RA synthase gene, was 2-fold higher in the BR group than the Cont group (P < 0.05).Conclusions
Brown rice prevented development of NAFLD in obese Zucker (fa/fa) rats. The beneficial effects of pregelatinized rice on NAFLD could be manifested as increased fatty acid oxidation and VLDL secretion, which are regulated by RA signaling.
https://www.sciencedirect.com/science/article/pii/S002231662200339X