Low Glutamate Diet
-
I've had better sleep and a steadier disposition since trying a low glutamate diet.
Gelatinous broth, gelatin, collagen, aged cheese, slow cooked meat, and anything with the "umami" flavor (like soy sauce) are high in glutamate. (Free glutamate, which is the issue.)
The low glutamate diet has been seen to help people with Autism, ADHD, OCD, Gulf War Syndrome.
-
@Insr said in Low Glutamate Diet:
The low glutamate diet
I'd take 0.5 g taurine.
useful info:
B6 PLP and taurine
To dampen glutamate's excitatory effects in the brain, the body converts it into the inhibitory neurotransmitter GABA (gamma-aminobutyric acid).
Pyridoxal 5'-phosphate (PLP), the active form of vitamin B6, is an essential cofactor for the enzyme glutamate decarboxylase (GAD), which catalyzes this conversion of glutamate to GABA.
Deficit in B6 when suffering from low-grade inflammation.
GABA helps maintain a healthy balance between neural excitation and inhibition. A deficiency in B6 can lead to reduced GABA synthesis and neuronal hyper-excitability. Mind the excess of B6 PLP (break). Do not use B6 PNP (neuropathy when above RDA). High doses of the vitamin B6 form pyridoxine (PN) can cause brain and nerve problems, though the primary effect is damage to peripheral nerves.
Taurine
The amino acids that can help dampen or balance glutamate activity include taurine, L-theanine, and the branched-chain amino acids (BCAAs).
0.5 g 2x/d.
NB: When I take L-glutamine (in case of thin linen stomach => acidity is painful), I balance with taurine. -
@LucH Thanks. For sleep and friendly calmness, I've found Theanine somewhat helpful, Taurine a little, and I didn't notice a benefit from P5P at either 50mg or 150mg.
Does anyone have an idea why I react to free glutamate in my diet? Most people can eat collagen or hot dogs and sleep fine

I've only noticed bad sleep and this irritated feeling in the last few years. Maybe 7 years ago I took collagen (high in glutamate) for a little while and found it to be soothing rather than irritating, as it's supposed to be. Maybe 4 years ago I took collagen again and didn't notice any effect at all. Now I get these excitotoxic effects from gelatinous broth (I haven't tried collagen) and actually from pure glycine too. (Glycine and Glutamate are the two NMDA receptor activators apparently)
Pregnenolone (which I've only tried this year) also gives me insomnia, which I understand is due to it going down the NMDA activating route as described here: https://lowtoxinforum.com/threads/is-insomnia-from-pregnenolone-common.43311/#post-719290
My cortisol tested just a little higher than the reference interval as of late May 2025.
My best theory is that my gum inflammation (started about 7 years ago) has weakened my blood brain barrier, thus allowing excess glutamate to get into my brain.
-
@Insr said in Low Glutamate Diet:
My best theory is that my gum inflammation (started about 7 years ago) has weakened my blood brain barrier, thus allowing excess glutamate to get into my brain.
I'd target another issue before saying glutamate is travelling towards the brain. yes, glutamate is an excitatory molecule Not only. Question of balance.
Glutamate is the principal excitatory neurotransmitter of the central nervous system and the most abundant neurotransmitter in the brain. But it plays a major role in learning and memory and has thus has to be balanced to avoid overheat. Too much glutamate is considered as an excitotoxin and is associated in such diseases as Parkinson’s, Alzheimer’s and Huntington’s disease.So, now another point that should be considered as more likely: Bone broth is very rich in histamine (H3). Bone broth is rich in amino acids like proline, glycine, glutamine, arginine, and glutamate, derived from collagen breakdown. Histamine comes from the histidine in animal flesh. Particularly when the meat is packed. Mind tuna.
Dual Action: Histamine acts both on nerves (causing itch) and blood vessels (causing swelling/redness). Red pimps on the skin.
I can develop to show how to manage and give a link. -
@LucH Thanks. I was wondering about histamine too. But the fact that pure glycine gave me insomnia makes me think there's an NMDA problem, not just histamine.
But if you have the time I would certainly like to hear ideas on histamine management.

-
@Insr said in Low Glutamate Diet:
pure glycine gave me insomnia
Glycine hasn't been taken at the right time (too late, at the dinner near bedtime) or too much. possibility. Not sure. I explain.
Glycine could be caught in the GABA shunt pathway. Used by the microbiota.
GABA is not a preferred primary carbon source for most gut bacteria as growth is usually stronger on sugars or amino acids like glutamate. But when the main fuel is rationed or when an access route is blocked, an alternate pathway is used.
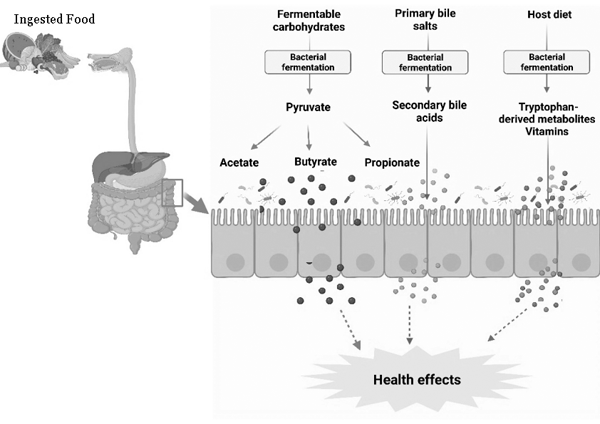
Glycine is use in the Gaba pathway.
Gaba => Succinate => butyrate pathway thanks to microbiota.
NB: I've asked confirmation from AI:
10g of glycine at dinner could influence the vagus nerve via microbiota and neurotransmitter pathways, as glycine interacts with GABA systems, and gut microbes process it, potentially affecting the gut-brain axis and vagal signaling, though high doses need caution and research suggests microbiota changes might be minimal, but the gut's glycine metabolism is key for brain availability.
Individual Variability: Glycine metabolism and microbiota response vary greatly; you might feel calming effects or potential digestive upset. Or just excitation when a food supply arrive for some bacteria.
I'd stop glycine for 10-15 days. Then take 1/3, but at midday.
Note, I'm making supposition. I'd better take magnesium bisglycinate. 1 g at breakfast and 1 g at midday. -
@Insr said in Low Glutamate Diet:
if you have the time I would certainly like to hear ideas on histamine management
How to deal with histamine intolerance
Addressing the root-cause of histamine intolerance
Most of the strategies for managing histamine intolerance prevent histamine from being either produced (histidine decarboxylase inhibitors) or released (mast cell stabilizers).
1st step: food
Managing a histamine intolerance tends to involve making dietary changes, taking antihistamines or enzyme supplements, and avoiding or limiting the use of some foods.
So, we are advised to reduce histamine levels by incorporating more low-histamine foods into our diet, such as fresh vegetables, fruits, and meats. Avoid or limit high-histamine foods, such as fermented products, aged cheeses, and processed meats.
Note that some foods don’t bring histamine (H1-3) but free histamine (L1-3). L stands for liberator.
For instance: canned tuna brings a high amount of histamine (H3), whereas orange fruit is a high liberator (L3). Citrus fruits don’t bring histamine but induce an allergic reaction in which histamine is freed.
2nd step: Help to get rid of excess- Useful nutrient for DAO enzyme: Namely Cu 1.5 mg.
- DAO supplement like NaturDAO. 1 000 000 Units
- Avoid DAO-Blocking Foods (like alcohol, tea and some nutraceutics, e.g. high B1)
- Support Your Gut Health (intolerance leads to immune reaction). Key point (dysbiosis).
- Balance Your Fat Intake (less omega-6, more omega-9 (olive oil), SFA is OK).[1]
- Methylation deficiency: 2 enzymes are required to deal with histamine: DAO and HNMT. HNMT = histamine N-methyltransferase. MTHFR polymorphism (gene defect) will make methylcobalamin supplement required (methyl-B12). HNMT transfers a methyl group (CH3) from S-adenosyl-L-methionine (SAM-e) to histamine, in order to inactivate / neutralize excess histamine. By degrading and regulating levels of intracellular histamine specifically within the CNS, HNMT ensures the proper functioning of neural pathways related to arousal, sleep-wake cycles, and other essential brain functions. To ensure adequate levels of HNMT enzymes, and Increase HNMT activity, a SAM-e supplement could be brought (as methyl donors).
Scientists have identified various nutrients that effectively boost DAO Enzymes levels. These nutrients include Omega-3 fatty acids, saturated fats, phosphorus, calcium, zinc, magnesium, iron, and vitamin B12.[1] Foods rich in these nutrients can help enhance DAO production. Help, not solve the problem.
3rd step: Calm down mastocytes
How to manage with release of various mast cell mediators. To lower excessive reaction.
For instance: - Quercetin anhydride. (Mind the kind). Once 500 mg a day. I take 2x 400 mg at the beginning, in crisis
- Herbal tea (gingimber and thyme + honey) in order to moderate theobromine (coffee, chocolate and especially tea) (=>methylxanthines such as theobromine and theophylline).
Sources and references
- Useful Info
- Dr. Becky Campbell – Free Histamine Guide.
- https://lowhistamineeats.com/clear-histamine-naturally/
- Reversing Histamine Intolerance Takes More Than a Low-Histamine Diet
https://caplanhealthinstitute.com/reversing-histamine-intolerance-takes-more-than-a-low-histamine-diet/ - https://drtaniadempsey.com/5-natural-antihistamines-to-combat-allergies/
- “Effect of dietary fatty acid and micronutrient intake/energy ratio on serum diamine oxidase activity in healthy women”
https://pubmed.ncbi.nlm.nih.gov/28606572/
Results: Serum DAO activity in both phases was positively correlated with intake of long-chain fatty acids, saturated fatty acids, and monounsaturated fatty acids (P < 0.05). Intake of phosphorus, calcium, zinc, magnesium, iron, and vitamin B12 during the luteal phase was positively correlated with serum DAO activity (P < 0.05). - “Nutrient-induced inflammation in the intestine – PMC –NCBI.”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4520304/
Understanding the relationship between nutrient absorption and intestinal inflammation is important. We need a better understanding of the interaction between enterocytes and the intestinal immune cells in nutrient absorption and the gut inflammatory responses. - The increased release of histamine and DAO is specific to fat feeding and is not shared by carbohydrate or protein feeding.
Wollin A, Wang XL, Tso P. Nutrients regulate diamine oxidase release from intestinal mucosa. Am J Physiol. 1998;275:R969–R975. [PubMed] [Google Scholar] - Adopting a leaky gut protocol or a diet rich in anti-inflammatory foods and high in antioxidants, can be instrumental in addressing the root-problem.
Improving gut health and taking DAO are pillars of histamine intolerance treatment.
https://caplanhealthinstitute.com/reversing-histamine-intolerance-takes-more-than-a-low-histamine-diet/
Useful nutrients include vitamins B6, copper, iron, magnesium, phosphorus, zinc, and vitamin C. (a,b) Each of these nutrients both support and modulate immune function for the better.
a. Maintz L, Novak N. Histamine and histamine intolerance. Am J Clin Nutr. 2007;85(5):1185-1196. doi:10.1093/ajcn/85.5.1185
b. Miyoshi M, Ueno M, Matsuo M, et al. Effect of dietary fatty acid and micronutrient intake/energy ratio on serum diamine oxidase activity in healthy women. Nutrition. 2017;39-40:67-70. doi:10.1016/j.nut.2017.03.004 - Le syndrome d'activation des mastocytes et l'activation inappropriée des mastocytes
Les symptômes proviennent principalement de la libération de médiateurs et comprennent un prurit, des bouffées de chaleur et une dyspepsie due à une hypersécrétion gastrique. - Mastocytes et inflammation
https://www.sciencedirect.com/science/article/abs/pii/S1169833012001615
L’importance de la fonction du mastocyte dans la réponse inflammatoire est mieux connue depuis quelques années. Son rôle dans certaines pathologies inflammatoires chroniques comme la polyarthrite rhumatoïde (PR) et la sclérose en plaque (SEP) montre l’importance de développer des thérapeutiques ciblant le mastocyte. L’efficacité des inhibiteurs de tyrosine kinase ciblant le récepteur c-Kit du mastocyte a déjà été démontrée dans plusieurs études, notamment dans la PR, l’asthme et la SEP.
-
@LucH Thank you for the info.