Important role of copper & vit D in schizophrenia (transporters) (Vitamin D and A / thyroid)
-
Copper looks to be highly significant in schizophrenia,
where blood levels can be higher than normal BUT brain levels lower in copper regardless (due to defective copper transport)so problem is with transport typically instead of levels, leading to functional deficiency in some brain areas at least:
ATP7A and B, and CTR1 are involved in copper transport
insightful studies
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6424639/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7987889/
These results provide the first evidence of disrupted copper transport in schizophrenia SN that appears to result in a copper-deficient state. Furthermore, copper homeostasis may be modulated by specific dysbindin isoforms and antipsychotic treatment.Interestingly, decreasing copper activity through by inhibiting transporters or administering the copper chelator cuprizone to mice produces demyelination, altered neurotransmitters, and decreased oligodendrocytic protein expression (Gokhale et al. 2015; Gregg et al. 2009; Herring and Konradi 2011). Additionally, reduced copper activity results in schizophrenia-like behavioural impairments, such as deficits in novel object recognition, spatial memory tasks, pre-pulse inhibition, social interaction, and anxiety
Additionally, schizophrenia patients exhibit decreased metallothionein and glutathione, responsible for intracellular copper chaperoning and transport, that are rescued with antipsychotic treatment (Xuan et al. 2015; Do et al. 2000)(Figure 1B)
In addition to those mentioned previously, lack of copper also exacerbates NMDA-mediated excitotoxic cell death in primary hippocampal neuronsGiven the excess of copper in the blood of schizophrenia patients and the increasingly mounting evidence of an abnormal or “leaky” BBB in psychosis, we hypothesize that schizophrenia patients exhibit excess blood copper due to faulty copper transport across the blood brain barrier (BBB). This abnormality would result in a copper-deficient brain state and contribute to the cognitive and behavioral deficits observed in schizophrenia. Our results suggest extracellular copper binding and transport into the cell via CTR1 is impaired in schizophrenia, and not rescued with treatment
when subdivided by medication status, the N-terminus [ATP7a] protein levels were significantly lower in unmedicated patients versus medicated patients (p=0.02) and controls
Analysis of treatment status revealed that C-terminal ATP7A protein levels were significantly increased only in medicated patients versus controls
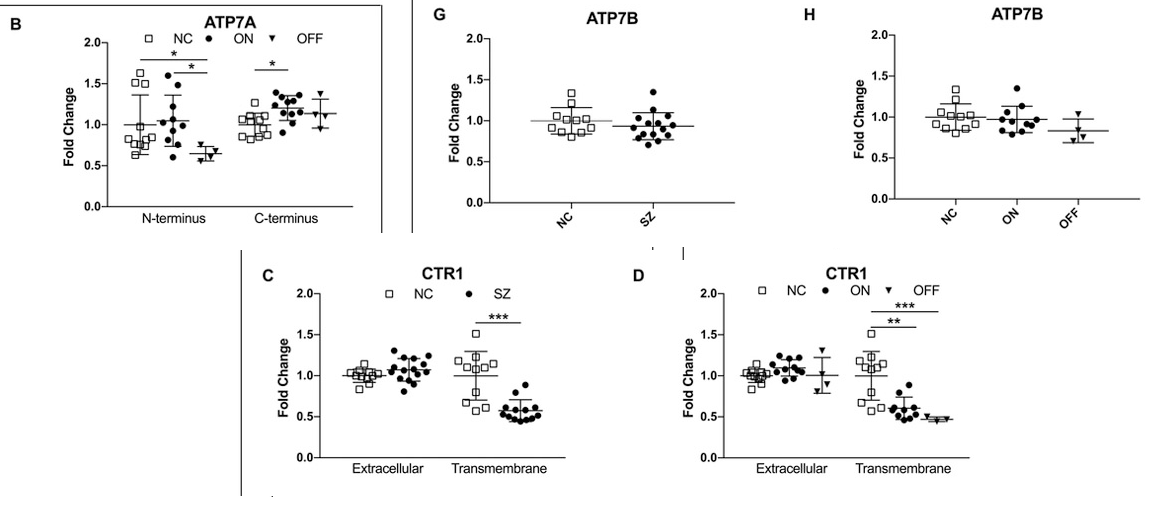
Copper transport proteins ^ ,people with schizophrenia not on medication have much lower n-terminus ATP7A expression. much lower transmembrane CTR1 expression. lower ATP7b expression.
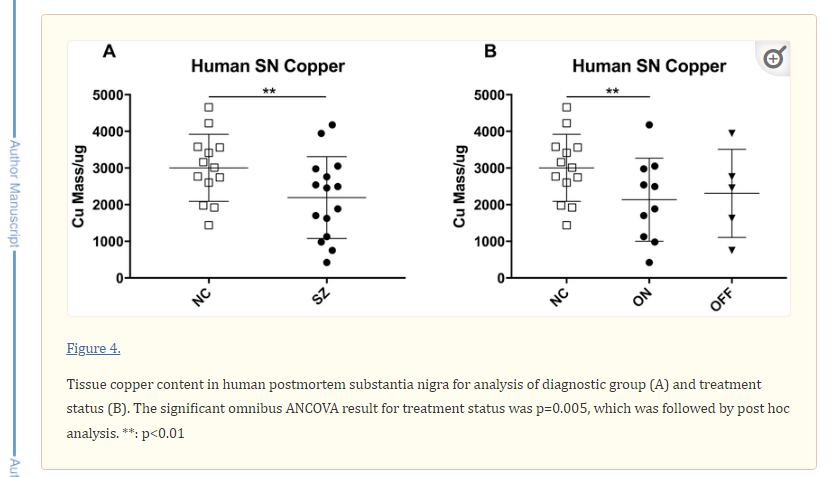
and less copper in the substantia nigra brain area tested for copper content[So this suggests another likely helpful area of focus is finding stuff that increases ATP7a and especially CTR1 expression]
3 basic things,
Vitamin A or thyroid hormone could help increase atp7a and vitamin D could help increase ctr1 (but need to be balanced)Interestingly there's been some mention of how schizophrenia has some commonalities with vitamin a excess or deficiency
(i) neurological congenital abnormalities reported in some schizophrenia cases are comparable to those observed with vitamin A deficiency or altered at-RA
(probably either deficiency or excess because like ive mentioned in another post, maybe overload could take away from vitamin D making CTR1 expression worse, where deficiency = not enough ATP7a)
https://www.nature.com/articles/s41380-019-0566-2#Sec7
^ intake of beta-carotene was demonstrated to be low in some schizophrenia cohortshttps://pubmed.ncbi.nlm.nih.gov/24434091/
^ here a synthetic vitamin a drug was used with positive effect in people with schizophreniatoo much vitamin A could skew things away from CTR1 more by countering vitamin D maybe. so personally i would like a closer ratio of vit D to A than normal considering importance of ctr1 here. maybe even 1:1 idk its guess work. beef liver is good source of vitamin A + copper
Thyroid hormone also increases ATP7a , needed for ceruloplasmin and exports copper from the liver (posted by youngsinatra before https://portlandpress.com/view-large/figure/2309956/bj4430103fig3.jpeg
& here's a great vitamin D effect in schizophrenia in humans
The psychotropic effect of vitamin D supplementation on schizophrenia symptoms(interestingly only 3.8% of people tested had vit d in normal range even though it was summer)
"Although our study population consisted of outpatients and blood samples were taken between May and July when sunlight is more intense, the rates of low vitamin D levels were found to be high"
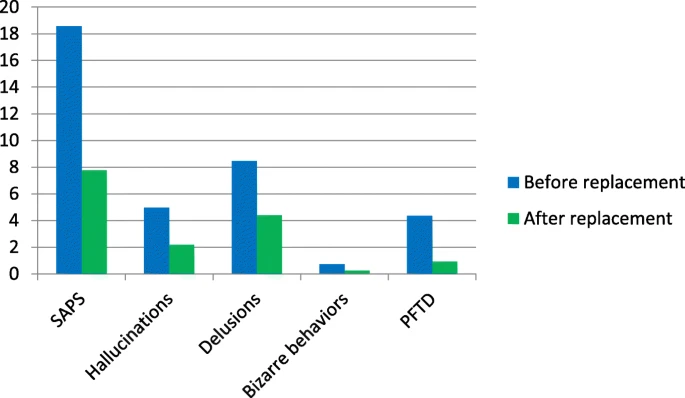 ^-- before & after vitamin D intake for 8 weeks. impressive effect size
^-- before & after vitamin D intake for 8 weeks. impressive effect sizeOur finding of decreased CTR1 in the cells and fibers of the superficial layers of the entorhinal cortex lends is consistent with the importance of copper in myelin integrity and dendritic spine formation, as well as cellular function. Deficits of myelin and associated oligodendrocytes have been well replicated in schizophrenia in several brain regions
Cortical areas exhibit decreased markers of myelin basic protein (a key component of myelin), fewer oligodendrocytes, abnormal oligodendrocyte morphology, oligodendrocyte degeneration, myelin thickness and laminar abnormalities, as well as downregulation of key myelin related genes and proteins in schizophrenia
Interestingly, application of the copper chelator cuprizone results in massive, albeit reversible, demyelination and oligodendrocyte death. indicating that copper must play a crucial role in myelin and oligodendrocyte function and integrity. If a deficit of cuprinergic signaling and copper content exists in the superficial layers of the entorhinal cortex in schizophrenia as indicated by our finding of decreased CTR1, this could impact white matter integrity in this area.
In contrast to our findings in the superficial layers of the entorhinal cortex, we observed significantly elevated immunolabeling of CTR1 in the molecular layer of the dentate gyrus, consistent with a trending increase of CTR1 mRNA within the middle temporal area
In further support of our suggestion of compensatory upregulation of CTR1 in the molecular layer of the dentate gyrus in response to copper deficit is the observation that the dentate gyrus exhibits deficient signalling in schizophreniaTaken together, our data suggest dysregulation of copper transport and homeostasis in the hippocampus and entorhinal cortex in schizophrenia that is region and layer specific, a potential mechanism of schizophrenia pathology that was previously unstudied. Deficient copper within the hippocampus could have deleterious effects, including decreased energy metabolism and neuronal signaling, deficits of myelin maintenance and integrity, and an overall pathological modulation of the trisynaptic pathway crucially involved in memory and cortical function {seen in alzheimers}
Therefore, further study is needed to assess cellular copper content and transporter status of each layer and cell type of the hippocampus in schizophrenia, as well as replication of the current study. Abnormal copper and other trace metals are becoming increasingly associated with schizophrenia and other forms of psychosis (Bitanihirwe and Cunningham, 2009; Joe et al., 2018; Schoonover et al., 2018) and therefore could provide a new mechanism to be targeted for development of better treatments. For instance, treatments that mimic the functions of CTR1 might enhance copper transport from the blood to the brain parenchyma could be therapeutic.
auditory dysfunction (hearing things) brain region:
In a comprehensive narrative review Hu et al. [30], summarized studies of glutamate neuron morphology, of the synthesizing and metabolizing enzymes for glutamate and its co-agonists and of the expression of glutamate transporters and receptors. They reported clear evidence in several regions, from multiple labs of reduced dendrite length and complexity and of lower levels of synaptophysin, a marker of axon boutons.
Additionally, reduced pyramidal somal volume has been found predominantly in layer III of dorsolateral prefrontal cortex (DLPFC) and auditory cortex. Hence, the dendrites, axons and cell bodies of cortical glutamatergic neurons are clearly reduced in size in schizophrenia.
www.nature.com
Reduced Pyramidal Cell Somal Volume in Auditory Association Cortex of Subjects with Schizophrenia - Neuropsychopharmacology
Subjects with schizophrenia have decreased gray matter volume of auditory association cortex in structural imaging studies, and exhibit deficits in auditory sensory memory processes subserved by this region. In dorsal prefrontal cortex (dPFC), similar in vivo observations of reduced regional...
www.nature.com www.nature.com^ the reduced volume in auditory cortex is mainly because of smaller cell size rather than fewer cell numbers
Volume decreases were found in 62% of 37 studies of whole temporal lobe, and in 81% of 16 studies of the superior temporal gyrus (and in 100% with gray matter separately evaluated). https://www.biologicalpsychiatryjournal.com/article/S0006-3223(99)00018-9/fulltext
so less gray matter volume of superior temporal gyrus of temporal lobe (where auditory cortex is), common to schizophrenia,
and seems the volume drop is mainly due to smaller cell size instead of fewer cells -
Very interesting, thank you for posting!