High DHEA, Cortisol, Prolactin and Cholesterol
-
@Kvirion Hi Kvirion, thank you for the detailed reply.
Yes I'm well known with Ray his work and had some succes, this is my fav quote of him "My recommendation is to eat to increase the metabloic rate (usually temperture and heart rate), rather than any particular foods..."
I have tried careful thyroid supplementation in the past, but without much success. I tried NDT from Lifegivingstore and T3 from Hilma. Both increased stress hormones too much even at low doses (3mcg T3), even with enough food, so I stopped. I also tried taking it with magnesium and salt, but had no luck. I only experienced rapid heart rate, cold hands, and feet from small doses. I tried it three times for two weeks, but saw no benefits; it only increased stress.
For now I only follow Danny's info and some of Hans.
My reverse T3 ratio to T3 seem perfect, it's 20.
@wester130 mentioned male pcos, my bloodwork matches with the elevated markers but only half of the symptoms PCOS - A Proposed Root Cause, I am not overweight or bald, but I'm only 29 but my problems started 15 years ago.
-
@StreamOfWater said in High DHEA, Cortisol, Prolactin and Cholesterol:
I have tried careful thyroid supplementation in the past, but without much success
What about trying to lower stress first?
With Royal jelly, theanine, or more advanced things like Aspirin, emodin (Cascara S.), or progesterone (Progest-E)? What about sun/red light, meditation, CO2, B vitamins, etc?PCOS - A Proposed Root Cause
Our body is an interconnected, nonlinear ecosystem, there is no singular "root cause".
Or as Nate nicely wrote:Health issues are not meant to be addressed directly. You heal by simply out-nourishing the issue. Until it feels like all aspects of your life are improving in unison, you are not adequately nourished. It should feel like nothing can break your stride. The bioenergetic symphony. ~@natelawrence_
-
@Kvirion Hi, I tried lowering stress far before I found peat his work, nothing worked and that is how I find out that I have subclinical hypothyroidism.
I also tried theanine, aspirin, cypro, progest-e (but I already have high progesteron) extra b vitamins but they lower stress only a little.
So I tried thyroid but that only increased the stress. I feel stuck.
-
@StreamOfWater said in High DHEA, Cortisol, Prolactin and Cholesterol:
So I tried thyroid but that only increased the stress. I feel stuck.
Sorry to hear that.
Have you tried to visit a doctor for a medical examination due to high cortisol? Or to consider things like for example Cushing disease?BTW do you know your estrogen/estradiol levels? Can't find it in the pictures attached...
https://raypeatforum.com/community/tags/cushings/
https://raypeat.com/articles/articles/hot-flashes-energy-aging.shtml -
@Kvirion I have been to my family doctor in the past for my symptoms but now had blood drawn myself and went to the family doctor with the results and he said everything looked good, that didn't help me at all and I am still angry about it.
I have not checked for estrogen/estradiol.
I will look into the links. Thank you.
-
@StreamOfWater Yeah, family doctors are usually simply trained to follow procedures and not "overthink".
I wouldn't trust the normal ranges on blood tests, they are just averages of results done by usually sick people...
There is a fascinating book about it https://drgabormate.com/book/the-myth-of-normal/BTW Regarding the cortisol test - a proper one should have morning and evening values... your doc screwed this up...
Vitamin D3 levels are also below optimal values...If I may suggest, it would be good to analyze your whole Hypothalamic–pituitary–adrenal axis - i.e. the main conductor of stress hormone synthesis...
Maybe you will discover which part of this axis makes trouble itself or is influenced by other parts of your body.
Your microbiota may also be problematic...Maybe such systemic analysis may help you get unstuck...
You may also look for Ray Peat's interviews about cortisol.
Moreover, also check Haidut's interviews about it https://www.youtube.com/results?search_query=georgi+dinkov+cortisol - he struggled with high cortisol himself and has excellent knowledge about it.You may also check this https://drgabormate.com/book/when-the-body-says-no/
-
@Kvirion Hi,
I conducted the blood test myself so I could select the markers based on recommendations from Ray and Danny. I took my blood at 8:30 AM, and based on my symptoms, my cortisol and adrenaline levels are often high. My vitamin D levels were indeed low, but I took 300,000 IU within a month, so that should be fine now.
I previously researched the HPA axis; it's quite complex. I ordered Cabergoline a few weeks ago (it still needs to arrive) and will try it to lower my prolactin levels. Perhaps it will help steer my health in the right direction.
If you want to know more about me you can just ask me. I appreciate your knowledge and assistance.
-
@BroJonas Sorry I missed your comment. Temp is 36.4c after waking up, later in the day 37.2c. Pulse is very low while relaxed, 45-55bpm. I don't do sports.
-
@StreamOfWater said in High DHEA, Cortisol, Prolactin and Cholesterol:
I conducted the blood test myself so I could select the markers based on recommendations from Ray and Danny. I took my blood at 8:30 AM, and based on my symptoms, my cortisol and adrenaline levels are often high. My vitamin D levels were indeed low, but I took 300,000 IU within a month, so that should be fine now.
This is good, maybe next time try morning and evening cortisol as this may be a useful diagnostic tool.
Wikipedia: "Studies on people show that the HPA axis is activated in different ways during chronic stress depending on the type of stressor, the person's response to the stressor, and other factors. Stressors that are uncontrollable, threaten physical integrity, or involve trauma tend to have a high, flat diurnal profile of cortisol release (with lower-than-normal levels of cortisol in the morning and higher-than-normal levels in the evening) resulting in a high overall level of daily cortisol release. On the other hand, controllable stressors tend to produce higher-than-normal morning cortisol. Stress hormone release tends to decline gradually after a stressor occurs. In post-traumatic stress disorder there appears to be lower-than-normal cortisol release, and it is thought that a blunted hormonal response to stress may predispose a person to develop PTSD.["
@StreamOfWater said
I previously researched the HPA axis; it's quite complex. I ordered Cabergoline a few weeks ago (it still needs to arrive) and will try it to lower my prolactin levels. Perhaps it will help steer my health in the right direction.
High prolactin is usually a symptom, not a cause. Cabergoline may offer some temporary relief, but most probably will not solve the key issues.
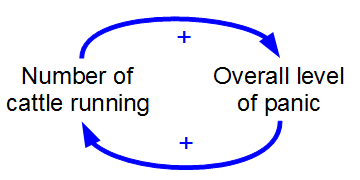
It would be good to consider that you may have some genetic sensitivity/proclivity for high stress (hormones). Plus you probably experienced some prenatal/childhood/adolescent (chronic/mild?) stress, which created mutually upregulating feedback loops... i.e. you may be in a permanent state of fight or flight mode... It may be hard to get out of it...
An optimal solution would be to address simultaneously biological, environmental, and psychological negative factors step-by-step.
You may start with a careful analysis of the following Wiki article, it's pretty
comprehensive and helpful... https://en.wikipedia.org/wiki/Hypothalamic–pituitary–adrenal_axis@StreamOfWater said
If you want to know more about me you can just ask me. I appreciate your knowledge and assistance.
Happy to help, I dealt with somewhat similar issues in the past. I know the hell/maze of doctors telling you that you're ok, but you are obviously not feeling right...
-
@Kvirion said in High DHEA, Cortisol, Prolactin and Cholesterol:
This is good, maybe next time try morning and evening cortisol as this may be a useful diagnostic tool.
I can do it, but it will not be soon because I need to check some other markers, and it's expensive. Adrenaline makes my extremities cold, but cortisol, which sometimes follows, will make my armpits smell bad, and I feel like it's damaging my body as a whole.
I understand that Prolactin is a symptom of my low thyroid function or high stress hormones. I did buy it to see if it can bring me some relief.
@Kvirion said in High DHEA, Cortisol, Prolactin and Cholesterol:
Plus you probably experienced some prenatal/childhood/adolescent (chronic/mild?) stress
I did. I had a much harder start than my brother (he is healthier). I had eye problems when I was born, my body had a hard time keeping the temperature up (born in winter), and my extremities often turned a little blue, around my lips and fingers. But around 10 years old I felt great, I know what good health feels like.
I will definitely look more into the HPA-axis. Something else that might be causing problems is my liver. I always had a hard time tolerating caffeine and alcohol; it always took much more time to eliminate them from my body. It also looks like that my liver has a problem storing glycogen, and that cortisol quickly kicks in to break down tissue to bring blood sugar up.
@Kvirion said in High DHEA, Cortisol, Prolactin and Cholesterol:
Happy to help, I dealt with somewhat similar issues in the past
I'm very happy for you that you are doing better. Did you dig yourself out of it?
-
@StreamOfWater said in High DHEA, Cortisol, Prolactin and Cholesterol:
and I feel like it's damaging my body as a whole.
Yep, low thyroid / high cortisol may cause muscle wasting, fat accumulation, etc.
also looks like that my liver has a problem storing glycogen
RAY PEAT: “Thyroid acting partly through the liver helps to lower prolactin production"
https://raypeat.com/articles/articles/hot-flashes-energy-aging.shtml "One of the things progesterone does is to stabilize blood sugar. In one experiment, hot flashes were found to be increased by lowering blood sugar and decreased by moderately increasing blood sugar (Dormire and Reame, 2003). Hypoglycemia increases brain hormones, corticotropin releases hormones, CRH (Widmaier, et al., 1988), which increases ACTH and cortisol. CRH causes vasodilation (Clifton, et al., 2005), and is more active in the presence of estrogen. Menopausal women are more responsive to its effects, and those with the most severe hot flushes are the most responsive (Yakubo, et al., 1990). | The first reaction to a decrease of blood glucose, at least in healthy individuals, is to increase the activity of the sympathetic nervous system, with an increase of adrenaline, which causes the liver to release glucose from its glycogen stores. The effect of adrenaline on the liver is very quick, but adrenaline also acts on the brain, stimulating CRH, which causes the pituitary to secrete ACTH, which stimulates the adrenal cortex to release cortisol, which by various means causes blood sugar to increase, consequently causing the sympathetic nervous activity to decrease. Even when the liver's glycogen stores are adequate, the system cycles rhythmically, usually repeating about every 90 minutes throughout the day."
Haidut: The methods for increasing glycogen storage depend very much on the specific organism/person, but if you are interested in trying some new things the first option I would suggest is to get some pure fructose (or fruit juices like apples that contain mostly fructose) and use that as your primary source of sugar for several days. Fructose is supposed to be particularly good at building up glycogen storage. | On the supplement side, taurine is supposed to help with that, but the dose varies wildly from person to person for optimal effects. So, you have to try to find out what works for you. Typically, effective doses are 2g-5g a day. | Another supplement that Peat wrote about is uridine. Read The Problem of Alzheimer's Disease as a clue to Immortality Part 1 | Finally, if you are interested in trying drugs (after consulting with your doctor of course) an older antihistamine and anti-acid drug famotidine (Pepcid) is exceptionally good at inhibiting glycogen breakdown and promoting the synthesis of new glycogen. It is worth noting that famotidine is unique in its glycogen effects among the anti-acid drugs and unlike other drugs it has no known interaction with any other drug or any known effects on liver health or metabolizing abilities. So, you could use that while loading up on sugar. Famotidine is helpful for several conditions completely unrelated to stomach acid such as schizophrenia and PTSD. A probable explanation of those benefits would be due to the drug improving glycogen storage/usage and thus improving brain energetic profile.
I'm very happy for you that you are doing better. Did you dig yourself out of it?

I spent a lot of time researching and healing my soul/psyche and body. I'm almost at the right spot, but the legal availability of some drugs (prescription only) is the thing I still need to overcome...