Substantively Lowered Levels of Pantothenic Acid (Vitamin B5) in Several Regions of the Human Brain in Parkinson's Disease Dementia
-
Substantively Lowered Levels of Pantothenic Acid (Vitamin B5) in Several Regions of the Human Brain in Parkinson's Disease Dementia
Abstract
Pantothenic acid (vitamin B5) is an essential trace nutrient required for the synthesis of coenzyme A (CoA). It has previously been shown that pantothenic acid is significantly decreased in multiple brain regions in both Alzheimer's disease (ADD) and Huntington's disease (HD). The current investigation aimed to determine whether similar changes are also present in cases of Parkinson's disease dementia (PDD), another age-related neurodegenerative condition, and whether such perturbations might occur in similar regions in these apparently different diseases. Brain tissue was obtained from nine confirmed cases of PDD and nine controls with a post-mortem delay of 26 h or less. Tissues were acquired from nine regions that show high, moderate, or low levels of neurodegeneration in PDD: the cerebellum, motor cortex, primary visual cortex, hippocampus, substantia nigra, middle temporal gyrus, medulla oblongata, cingulate gyrus, and pons. A targeted ultra-high performance liquid chromatography-tandem mass spectrometry (UHPLC-MS/MS) approach was used to quantify pantothenic acid in these tissues. Pantothenic acid was significantly decreased in the cerebellum (p = 0.008), substantia nigra (p = 0.02), and medulla (p = 0.008) of PDD cases. These findings mirror the significant decreases in the cerebellum of both ADD and HD cases, as well as the substantia nigra, putamen, middle frontal gyrus, and entorhinal cortex of HD cases, and motor cortex, primary visual cortex, hippocampus, middle temporal gyrus, cingulate gyrus, and entorhinal cortex of ADD cases. Taken together, these observations indicate a common but regionally selective disruption of pantothenic acid levels across PDD, ADD, and HD.
https://pubmed.ncbi.nlm.nih.gov/34564384/Localized Pantothenic Acid (Vitamin B5) Reductions Present Throughout the Dementia with Lewy Bodies Brain
Abstract
Background: Localized pantothenic acid deficiencies have been observed in several neurodegenerative diseases such as Alzheimer's disease (AD), Parkinson's disease dementia (PDD), and Huntington's disease (HD), indicating downstream energetic pathway perturbations. However, no studies have yet been performed to see whether such deficiencies occur across the dementia with Lewy bodies (DLB) brain, or what the pattern of such dysregulation may be.Objective: Firstly, this study aimed to quantify pantothenic acid levels across ten regions of the brain in order to determine the localization of any pantothenic acid dysregulation in DLB. Secondly, the localization of pantothenic acid alterations was compared to that previously in AD, PDD, and HD brains.
Methods: Pantothenic acid levels were determined in 20 individuals with DLB and 19 controls by ultra-high performance liquid chromatography-tandem mass spectrometry (UHPLC-MS/MS) across ten brain regions. Case-control differences were determined by nonparametric Mann-Whitney U test, with the calculation of S-values, risk ratios, E-values, and effect sizes. The results were compared with those previously obtained in DLB, AD, and HD.
Results: Pantothenic acid levels were significantly decreased in six of the ten investigated brain regions: the pons, substantia nigra, motor cortex, middle temporal gyrus, primary visual cortex, and hippocampus. This level of pantothenic acid dysregulation is most similar to that of the AD brain, in which pantothenic acid is also decreased in the motor cortex, middle temporal gyrus, primary visual cortex, and hippocampus. DLB appears to differ from other neurodegenerative diseases in being the only of the four to not show pantothenic acid dysregulation in the cerebellum.
Conclusions: Pantothenic acid deficiency appears to be a shared mechanism of several neurodegenerative diseases, although differences in the localization of this dysregulation may contribute to the differing clinical pathways observed in these conditions.
Plain language summary
Decreases in a molecule called pantothenic acid (also known as vitamin B5) have been observed in several areas of the brain in multiple dementia disease, including Alzheimer’s disease, Parkinson’s disease dementia, and Huntington’s disease. However, it is unknown whether such changes also occur in another dementia disease, dementia with Lewy bodies, which shows many of the same symptoms and molecular changes as these conditions. As such, this study was performed in order to determine if and where changes in pantothenic acid occur throughout the dementia with Lewy bodies brain. Using a methodology called liquid chromatography–mass spectrometry, which is able to measure pantothenic acid levels in a highly precise manner in brain tissues, we found that several regions of the dementia with Lewy bodies brain show decreases in pantothenic acid, including some involved in movement such as the substantia nigra and motor cortex, as well as regions associated with cognition and memory such as the hippocampus—looking most similar to the pattern of changes already seen in Alzheimer’s disease. It is possible that these changes contribute to the progression of dementia with Lewy bodies; however, further studies need to be performed to determine at what point these changes happen during the disease and how they may contribute to the development of symptoms. -
@AlphaCog - Thanks, it is interesting that low levels of B5 is involved with several types of dementia. Increasing dietary levels of B6, B9 and B12 to lower homocysteine is a better known association for lowering ones risk of dementia.
Homocysteine, Cognitive Functions, and Degenerative Dementias: State of the Art (2022)
I found the article below interesting. B5 is discussed at pages 9-10.
B Vitamins and Fatty Acids: What Do They Share with Small Vessel Disease-Related Dementia? (2019)
-
Its name comes from the Greek πάντοθεν pantothen, meaning "from everywhere", because pantothenic acid, at least in small amounts, is in almost all foods. Deficiency of pantothenic acid is very rare in humans.
https://en.wikipedia.org/wiki/Pantothenic_acidFrom this we infer that people with dementia probably had poor digestion.
Gastrointestinal Diseases, Genetic Risk, and Incident Dementia: A Prospective Cohort Study in 352,463 Middle-Aged Adults
Conclusions and relevance This study found associations of several gastrointestinal diseases with an increased risk of incident dementia, especially early-onset dementia. Our findings imply the great importance of dementia prevention among patients with gastrointestinal diseases.
https://www.medrxiv.org/content/10.1101/2022.11.28.22282820v1.fullDementia with Lewy bodies (DLB) patients suffer more frequently from gastrointestinal dysfunction
https://wfneurology.org/activities/news-events/archived-news/2017-09-18-wcn-dlb-patients-suffer-more-from-gastrointestinal-dysfunctionDysbiosis, gut barrier dysfunction and inflammation in dementia: a pilot study
https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-020-01644-2 -
@AlphaCog most b5 production might be produced in the gut instead of from food, aligning with those studies (which would make rda irrelevant)
i think the impact here is on need to help myelin repair so brain can function well
its a nice finding theres an intervention study showing effects on mammals in alzheimers model, https://link.springer.com/article/10.1007/s13311-019-00754-z#Sec12 the amyloid-β idea is apparently based on fraud, but shows b5 lowering the excess aggression & restoring neuroinflammation to controls
Vitamin B5 (d-pantothenic acid) localizes in myelinated structures of the rat brain: Potential role for cerebral vitamin B5 stores in local myelin homeostasis
https://pubmed.ncbi.nlm.nih.gov/31759626/ -
-
@cs3000 said in Substantively Lowered Levels of Pantothenic Acid (Vitamin B5) in Several Regions of the Human Brain in Parkinson's Disease Dementia:
@AlphaCog most b5 production might be produced in the gut instead of from food, aligning with those studies (which would make rda irrelevant)
I developed Parkinson's last year out of carelessly taking orally cinnamon bark essential oil without the use of a capsule. I instead used sugar cubes, which may have needlessly exposed my gut to a substance which eradicated some valuable gut bacteria, probably impairing my gut's ability to absorb certain b-vitamins vital for peripheral motor nerve coordination.
This study speaks more to the use of b vitamins together with the intake of probiotics, which has the effect of facilitating the absorption of b vitamins thru the action of certain probiotic gut bacteria.
https://pubs.rsc.org/en/content/articlelanding/2024/fo/d4fo01805b/unauth
Abstract
B vitamins and probiotics are commonly used dietary supplements with well-documented health benefits. However, their potential interactions remain poorly understood. This study aims to explore the effects and underlying mechanisms of the combined use of B vitamins and probiotics by liquid chromatography-triple quadrupole mass spectrometry analysis, pharmacokinetic modeling, and 16S rRNA gene sequencing. By intragastric administration of seven B vitamins and three Lactobacillus strains to healthy rats (n = 8 per group), we found that probiotics significantly promoted the absorption (by approximately 14.5% to 71.2%) of vitamins B1, B3, B5, and B12. By conducting in vitro experiments (n = 3 per group) and a pseudo-germ-free rat model-based pharmacokinetic study (n = 6 per group), we confirmed that probiotics primarily enhanced the B vitamin absorption through gut microbiota-mediated mechanisms, rather than by directly producing B vitamins. Furthermore, we evaluated the effects of B vitamins and probiotics on the colon and gut microbiota by treating the pseudo-germ-free rats with blank solution, B vitamins, probiotics, and B vitamins + probiotics (n = 5 per group), respectively. Histopathological examination showed that the combination of B vitamins and probiotics synergistically alleviated the rat colon damage. High-throughput genetic sequencing also revealed the synergistic effect of B vitamins and probiotics in modulating the gut microbiota, particularly increasing the abundance of Verrucomicrobia and Akkermansia. In summary, the combined administration of B vitamins and probiotics may have a higher efficacy than using them alone. -
@yerrag maybe played a role, and also directly as cinnamon has some nasty effects
it can drop cholesterol (also needed for myelin in the brain) + crash T3 levels
https://diabetesjournals.org/care/article/26/12/3215/21858/Cinnamon-Improves-Glucose-and-Lipids-of-People
1g 3g 6g all reduce cholesterol , These decreases in serum cholesterol level ranging from 13 to 26% were maintained even after not consuming additional cinnamon for 20 days
maybe partly due to a buildup of benzoate over weeks which has toxicity at a certain level and takes a while to leave systemhttps://pubmed.ncbi.nlm.nih.gov/26374392/
** LOWERS T3 ACTION IN HEART AT 4G WATER EXTRACT 25 DAYS (lower trA mrna and protein levels) and LOWERED SERUM T3(heart toxic)
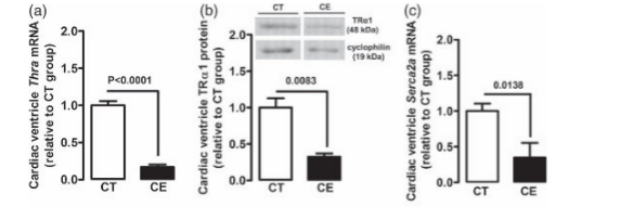
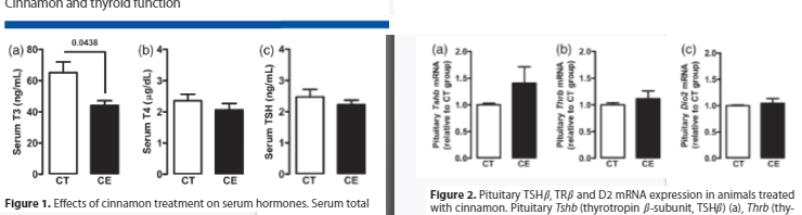
https://www.sciencedirect.com/science/article/pii/S1756464618305139 4g of cinnamon powder crashed t3 the same as extract
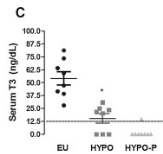
Interestingly, the treatment with cinnamon, in both preparations, further reduced serum T3 of hypothyroid animals to undetectable levels
-
@cs3000 thankfully the amount of toxicity I got from cinnamon is limited so it didn't impact my thyroid as much and I'm still euthyroid.
But I may not be affected at the gut level as much as at the brain and spine level thinking about it. It seems that my gut would be any less affected had I taken the cinnamon oil with a capsule instead of a sugar cube.
It is more likely that my myelin sheath is exposed and causing my Parkinsonian symptoms. But it is more a result of oxidative stress from free iron destroying the myelin membrane, a result of heme oxygenase releasing iron from red dead blood cells, with red blood cells dying en masse from oxygen starvation when I was having bronchitis, due to cinnamon bark oil exposure.
-
Pantethine
Because of pantothenic acid’s role in triglyceride synthesis and lipoprotein metabolism, experts have hypothesized that pantothenic acid supplementation might reduce lipid levels in patients with hyperlipidemia [19].Several clinical trials have shown that the form of pantothenic acid known as pantethine reduces lipid levels when taken in large amounts [20], but pantothenic acid itself does not appear to have the same effects [1]. A 2005 review included 28 small clinical trials (average sample size of 22 participants) that examined the effect of pantethine supplements (median daily dose of 900 mg for an average of 12.7 weeks) on serum lipid levels in a total of 646 adults with hyperlipidemia [20]. On average, the supplements were associated with triglyceride declines of 14.2% at 1 month and 32.9% at 4 months. The corresponding declines in total cholesterol were 8.7% and 15.1%, and for low-density lipoprotein (LDL) cholesterol were 10.4% and 20.1%. The corresponding increases in high-density lipoprotein (HDL) cholesterol were 6.1% and 8.4%.
A few additional clinical trials have assessed pantethine’s effects on lipid levels since the publication of the 2005 review. A double-blind trial in China randomly assigned 216 adults with hypertriglyceridemia (204–576 mg/dl) to supplementation with 400 U/day CoA or 600 mg/day pantethine [21]. All participants also received dietary counseling. Triglyceride levels dropped by a significant 16.5% with pantethine compared with baseline after 8 weeks. Concentrations of total cholesterol and non-HDL cholesterol also declined modestly but significantly from baseline. However, these declines might have been due, at least in part, to the dietary counseling that the participants received.
Two randomized, blinded, placebo-controlled studies by the same research group in a total of 152 adults with low to moderate cardiovascular disease risk found that 600 mg/day pantethine for 8 weeks followed by 900 mg/day for 8 weeks plus a therapeutic lifestyle change diet resulted in small but significant reductions in total cholesterol, LDL cholesterol, and non-HDL cholesterol compared with placebo after 16 weeks [19,22]. Increasing the amount of pantethine from 600 to 900 mg/day did not increase the magnitude of reduction in the lipid measures.
Additional studies are needed to determine whether pantethine supplementation has a beneficial effect on hyperlipidemia independently of, and together with, eating a heart-healthy diet. Research is also needed to determine the mechanisms of pantethine’s effects on lipid levels.
https://ods.od.nih.gov/factsheets/PantothenicAcid-HealthProfessional/#h9