Hyperinsulinemia and Its Pivotal Role in Aging, Obesity, Type 2 Diabetes, Cardiovascular Disease and Cancer
-
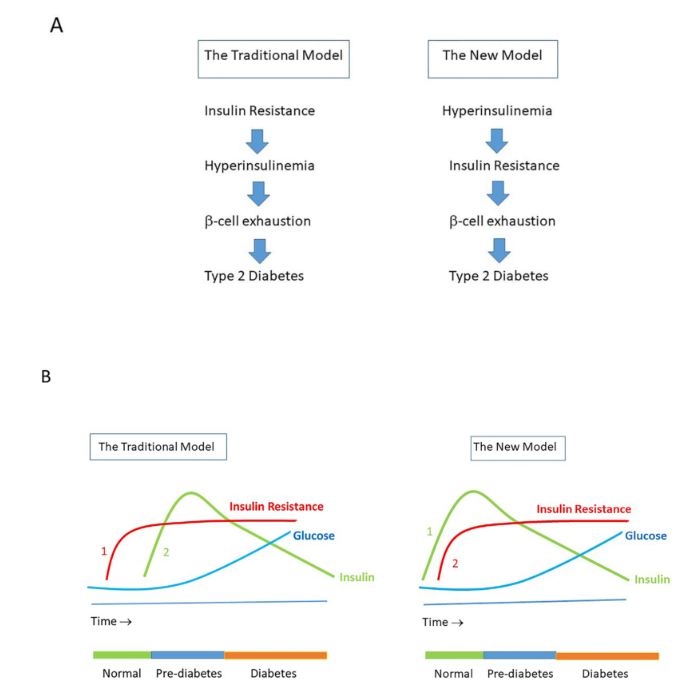
Hyperinsulinemia, driven largely by a junk food diet (and being sedentary), greatly increases the risk of all modern chronic diseases.
It also accelerates aging.

-
This post is deleted! -
This is a sounder model, but that's all it is as it is only less sound.
How the medical system has put insulin at the apex of its medical malfeasance dogma is appalling, along with its many falsehoods. To name a few more equivalents of Nobel laureate level hoaxing such as the banshee worship of non-existent viruses, the bedevelling of CO2 within and without the body (downplaying its salutary role as an all important pH buffer within, and its regulatory role in providing earth with a green blanket of forests), the vilification of protective hormones such as progesterone with the false worship of estrogen in its altar of repose with western christian churches in an evil collaboration of promoting superstition and fear.
Even the bioenergetic community blathers on the term insulin resistance as it echoes in unison with the false reliance on insulin as it's savior, refusing to see insulin as just another stress hormone from the true Peatarian view of it. Instead of less insulin being seen as beneficial, insulin is viewed as needed and vital to blood sugar regulation.
To such extent that when the body refuses to lower blood sugar as the charlatans would have us believe, it is never called an acute phase biomarker but instead the body is considered stupid and unwise and in dysregulation.
Insulin does more than just lower blood sugar, and it only does so when the body's ability to absorb and metabolize sugar efficiently via the mitochondria. Only when the body fails in lowering blood sugar does insulin step in. And in corrective fashion, when it tells the liver to convert excess blood sugar to fat.
But when the body is doing well in absorbing and metabolizing sugar, with little or no help from insulin, there is just a minimum level of insulin around that is keeping insulin from inhibiting other metabolic pathways such as lipolysis (as well as other processes which space and the interest of brevity does not permit).
Lipolysis being uninhibited is wrongly viewed as evil from the false notion that there is forum consensus of fat or beta-metabolism as being unequivocally unsound. This is a mental block which keeps most Peatarians from really achieving metabolic health.
Why would inhibiting lipolysis be a bad idea, I ask? For one, how would you lose weight when you don't convert fat cells into fatty acids for these fatty acids to be used as a substrate for producing energy in the mitochondria?
Couple this with the inane idea that more insulin is needed as the solution to lowering your blood sugar, according to mainstream medical thought and experts, not on the strength of evidence but on the usual Nobel Prize-level of propaganda and hoaxing and insulting of our intelligence with Pied Pipers of long noses where we only see long noses as normal only because our de facto religion sanctifies long noses.
Without realizing that an overabundance of insulin not only keeps fat stores in stasis, as we keep our overweightness and obeseness fully intact; while at the same time our liver is told by insulin to tack on more weight by converting blood sugar to fat, and the obvious outcome would be weight gain and poor health.
And then we are mad at United Healthcare for being the proverbial hitman for the lying pharma complex for denying us treatment from being so sick from stupidly taking hook line and sinker pharma's obvious lies as we descend into metabolic hell.
-
That general view of some peaters about lipolysis that you quoted in your reply probably stems from a misinterpretation of what Ray said about it. The emphasis he places on inhibiting lipolysis is in the context of too much PUFA stored in the tissues, which becomes less and less necessary as you become “PUFA depleted”. After that, inhibiting lipolysis becomes more of a therapeutic tool to be used in appropriate contexts, such as in some pathologies.
He even mentions that in healthy people (especially children) stress hormones are only produced in the amount needed because free saturated fatty acids serve as negative feedback, not allowing them to rise beyond what is necessary.
In good health, especially in children, the stress hormones are produced only in the amount needed, because of negative feedback from the free saturated fatty acids, which inhibit the production of adrenalin and adrenal steroids, and eating protein and carbohydrate will quickly end the stress. But when the fat stores contain mainly PUFA, the free fatty acids in the serum will be mostly linoleic acid and arachidonic acid, and smaller amounts of other unsaturated fatty acids. These PUFA stimulate the stress hormones, ACTH, cortisol, adrenaline, glucagon, and prolactin, which increase lipolysis, producing more fatty acids in a vicious circle. In the relative absence of PUFA, the stress reaction is self limiting, but under the influence of PUFA, the stress response becomes self-amplifying.
This misinterpretation is probably one of the bases for the idea that moderately high insulin several times a day is beneficial (because it inhibits lipolysis and increases glucose oxidation). I don't particularly consider insulin to be a “stress hormone”, but high insulin several times a day and for long periods is obviously a bad sign; insulin plays an “enhancing” role and not the main role.
Keto diets, a very low fat and/or very low protein diet, exercise, ACV before meals, walking after meals, and other similar tools aimed at reducing insulin are only necessary if metabolic dysfunction is already present. Is it good to have these options available with the constant attacks on our health? Yes, but the more miraculous a therapeutic tool is, the more likely it is that your health isn't as good as you think.
-
@TexugoDoMel said in Hyperinsulinemia and Its Pivotal Role in Aging, Obesity, Type 2 Diabetes, Cardiovascular Disease and Cancer:
That general view of some peaters about lipolysis that you quoted in your reply probably stems from a misinterpretation of what Ray said about it. The emphasis he places on inhibiting lipolysis is in the context of too much PUFA stored in the tissues, which becomes less and less necessary as you become “PUFA depleted”. After that, inhibiting lipolysis becomes more of a therapeutic tool to be used in appropriate contexts, such as in some pathologies.
I agree with how you qualify the need for inhibition of lipolysis, in that it is only needed when there is too much PUFA stored in the tissues.
When that is the case, inhibiting lipolysis to such extent that fat stores don't undergo lipolysis except for a trickle isn't the solution, as when one takes too much niacinamide or when one increases insulin levels either by injection or by excreting a lot of it. As this keeps fat stores abundant and the person overweight or obese, and goes against the objective of becoming of normal weight again.
The answer lies in going cold turkey on further intakes of PUFA for a relatively long period of time, say about 4 years, during which time PUFA stores are allowed to slowly lipolyze. During this time, PUFA will be released from fat stores and so the stress it produces has to be minimized. Because the presence of PUFAs is expected to hinder sugar absorption and metabolism, there is no choice but to accept that as a transitionary evil to be dealt with. It would be helpful to take antioxidants such as vitamin E to minimize runaway lipid peroxidation reactions and to minimize blocks in the ETC arising from lipid peroxidation, and to modify food intake by eating carbs that have fiber that slow down the time and the rate by which carbs are assimilated into the blood stream. Instead of a quick sudden flood of glucose from eating white rice, eating brown rice would help slow the flow of blood sugar to a trickle that doesn't overwhelm the limited rate by which the body absorbs blood sugar. This keeps blood sugar from rising too much that triggers the release of insulin which often results in blood sugar being converted to fat in the liver and in blood sugar dropping to very low levels, which causes stress to increase from low blood sugar levels.
Accompanying the brown rice with plenty of meat protein and some fat in that meal would further slow down the rate of assimilation of sugar into the blood stream. In this way, blood sugar from a meal would trickle is slowly over a longer period of time. Ideally, the rate it trickles in would keep blood sugar maintained at normal healthy levels from that meal well into the next meal without blood sugar getting too high nor too low. Managing to achieve blood sugar stability between meals would keep the body from having to increasing insulin levels. Without high insulin levels, the body would be allowed to lose fat by lipolysis over this period while it is kept from making more fats via insulin signaling (with insulin being kept from being excreted excessively from minimizing high blood sugar levels).
This is not an easy task, as 4 years in a long time, and requires one to have the discipline to stick to the plan. With patience, over time the body will be rid of PUFAs, and this will open the way for blood sugar to be quickly absorbed and metabolized.
One can eat white rice once again, and as the ability to metabolize sugar optimally via the mitochondria is restored and strengthened, basal metabolism improves to such extent that internal metabolism increases, making the need for external metabolism less needed.
One can eat plenty of white rice with no need to do any tricks like intermittent fasting and have no need to walk the stupid 10,000 steps a day to be slim and normal weighted. Like I do.
Which is why I fail to see the wisdom in people saying one can bypass the 4-year cold turkey on PUFA intake by simply taking niacinamide and aspirin. This method just keeps PUFA in the fat stores and minimizes beta oxidation and the conversion of fatty acids into energy.
Moreover, relying on insulin excretion is only useful in lowering blood sugar st the cost of gaining weight. Which explains why following the dictates of the AMA and their doctors is a surefire way for the country to have an obesity epidemic and for the health of the population to keep getting worse.
For such a population, healthcare insurance companies can only make money by denying treatment as an insurance system where 100 percent of those insured will get sick and need costly treatment. When treatment is guaranteed for the sick, the healthcare insurance company will just go broke.
He even mentions that in healthy people (especially children) stress hormones are only produced in the amount needed because free saturated fatty acids serve as negative feedback, not allowing them to rise beyond what is necessary.
Good point. I must have missed reading this. Could you share the newsletter or where it is quoted?
In good health, especially in children, the stress hormones are produced only in the amount needed, because of negative feedback from the free saturated fatty acids, which inhibit the production of adrenalin and adrenal steroids, and eating protein and carbohydrate will quickly end the stress. But when the fat stores contain mainly PUFA, the free fatty acids in the serum will be mostly linoleic acid and arachidonic acid, and smaller amounts of other unsaturated fatty acids. These PUFA stimulate the stress hormones, ACTH, cortisol, adrenaline, glucagon, and prolactin, which increase lipolysis, producing more fatty acids in a vicious circle. In the relative absence of PUFA, the stress reaction is self limiting, but under the influence of PUFA, the stress response becomes self-amplifying.
This misinterpretation is probably one of the bases for the idea that moderately high insulin several times a day is beneficial (because it inhibits lipolysis and increases glucose oxidation). I don't particularly consider insulin to be a “stress hormone”, but high insulin several times a day and for long periods is obviously a bad sign; insulin plays an “enhancing” role and not the main role.
Keto diets, a very low fat and/or very low protein diet, exercise, ACV before meals, walking after meals, and other similar tools aimed at reducing insulin are only necessary if metabolic dysfunction is already present. Is it good to have these options available with the constant attacks on our health? Yes, but the more miraculous a therapeutic tool is, the more likely it is that your health isn't as good as you think.
If we peel away the layers of band aid we rely on, we realize that is the standard of care that only leads to the creation of more problems that require our experts in the medical establishment to guide us to the promised land.