High-dose thiamine troubleshooting
-
@mostlylurking said in High-dose thiamine troubleshooting:
Please tell me what is "MMC"
The migrating motor complex (MMC) is an electrical and contractile activity of digestive motility which takes place in the inter-digestive periods (between two meals), and interrupted by food intake. Each MMC is accompanied by an increase in gastric, pancreatic and duodenal secretions. They are thought to serve to evacuate contents in the small intestine between meals, and also to transport bacteria from the small intestine into the colon. An alteration of this phase notably favors the development of chronic bacterial colonization of the small intestine, a source in particular of bloating, diarrhea, or even steatorrhea, of the majority of food intolerances. When contractile activity is low, we then speak of lazy intestines. Support and rehabilitation is often necessary, with a prokinetic (Resolor 0.5 mg), initially.
-
@LucH said in High-dose thiamine troubleshooting:
@mostlylurking said in High-dose thiamine troubleshooting:
Please tell me what is "MMC"
The migrating motor complex (MMC) is an electrical and contractile activity of digestive motility which takes place in the inter-digestive periods (between two meals), and interrupted by food intake. Each MMC is accompanied by an increase in gastric, pancreatic and duodenal secretions. They are thought to serve to evacuate contents in the small intestine between meals, and also to transport bacteria from the small intestine into the colon. An alteration of this phase notably favors the development of chronic bacterial colonization of the small intestine, a source in particular of bloating, diarrhea, or even steatorrhea, of the majority of food intolerances. When contractile activity is low, we then speak of lazy intestines. Support and rehabilitation is often necessary, with a prokinetic (Resolor 0.5 mg), initially.
Thanks. I wasn't familiar with the term and searching for "MMC" yields all kinds of stuff that is not possibly pertinent. Even searching for "MMC medical" yields a plethora of obviously inapplicable results.
Gut motility and its control
"Smooth muscle cells in the GI tract are bundled together and are linked by gap junctions that allow the flow of electrical signals between the cells, allowing them to contract as a functional syncytium. Control of the muscles, and thus gut motility, is complex and is co-ordinated by the autonomic nervous system, hormones and other mechanisms intrinsic to the GI tract. In this way, the GI tract is able to respond to changes in the luminal environment caused by food intake."also this one:
"Central nervous control of the MMC. Currently, there
is no doubt that the nervous control of the MMC is crucial for its initiation and modulation. It comprises the evident neural responses due to neuromediator’s action and interplay among NANC-related central and peripheral modulators as well as the hormones (principally peptide hormones) [3, 4]. Central nervous control of the stomach and small intestine comprises mainly the effects mediated by extrinsic innervation of these regions, i.e. vagal and sympathetic nerve-related influences (Fig. 1). These actions mediated by the efferent nerves occur as the response to central effects and peripheral (afferent) stimuli from the gastrointestinal tract. One of the incompletely resolved questions is: what is the precise role of the central effects vs. the peripheral nervous influences in the control of the MMC cycle? There is increasing knowledge focusing on the role of the central nervous system in the control of the MMC that comprises the scientific evidence derived from physiological, pharmacological, surgical and clinical experiments and observations."How Can Something As Simple as Thiamine Cause So Many Problems?
"The lower part of the brain, called the brainstem, is a like computer, controlling the most basic aspects of survival, from breathing and heart rate, hunger and satiety, to fight or flight and reproduction. This computer-like function within the brainstem is called the autonomic system (ANS). The ANS together with the limbic system act in concert to regulate our most basic survival functions and behaviors. Both require thiamine to function."Here's a video from EONutrition:
Is Thiamine Deficiency Destroying Your Digestive Health? Why B1 Is ESSENTIAL For Gut Function -
@LucH said in High-dose thiamine troubleshooting:
Support and rehabilitation is often necessary, with a prokinetic (Resolor 0.5 mg), initially.
about Resolor:
"How does Resolor work? The active substance in Resolor, prucalopride, is a ‘5-HT4 receptor agonist’. This means that it works like a substance in the body called 5-hydroxytryptamine (5-HT, also known as serotonin) and attaches to receptors for 5-HT in the gut called ‘5-HT4 receptors’.When 5-HT binds to these receptors, it normally stimulates movement in the gut. In the same way, when prucalopride attaches to and stimulates these receptors, it increases this movement and allows the bowels to empty faster."
Ray Peat on serotonin:
Serotonin, depression, and aggression: The problem of brain energyWhen I was thiamine deficient, I was extremely sensitive to serotonin. This was probably because thiamine is needed to clear serotonin from the brain. Taking something that increases serotonin when thiamine deficient is not something I would do.
Effect of thiamine deficiency on brain serotonin turnover -
@mostlylurking
I agree with your analyze on excess serotonin and 5-HTP (targeting SSRI, thus increasing central nervous system synthesis of serotonin).
SSRI = Selective Serotonin Reuptake Inhibitor.
Saying that, prucalorid is taken, not as a laxative – at the usual dose of 2 mg – but as a stimulus (0.5 mg resolor). The dose is very weak but sufficient for re-educating a lazy gut.
Here we’re trying to find a solution for colonic motility dysfunction. And the solution has not to be found with a laxative. This is not because of a lack of electrolytes, fibbers or exercises. By the way, 30 grams fibbers is needed, with soothed fibbers (progressive).
When suffering from insufficient electrical contractile bowel movements, between 2 meals, we aren’t targeting a problem of transit. The muscle contractions are called peristalsis. This process must be re-educated. Of course, the IBS problem (high-amplitude propagating contractions) must be taken into account. First calming down irritation, afterwards stimulation of the stasis.
Note that when I took resolor 0.5 mg, I took it 2 hours before bedtime (3-4 days adaptation period).
A box of 28 tablets cut into two parts = 56 days of treatment (cut with a sharp kitchen knife). No need for a second box.
Once a day for stools wasn’t enough to get rid of excess / unbalanced intestinal bacteria. Some bacteria had nothing to do in the second part of the colon.
The problem in now under control, with the help of diamine oxidase. Too much histamine. (NaturDAO, 1 000 000 units).
Note: The warning concerns the usual employment to a high dosage of 5-HTP and against an excess of serotonin. The excesses are obviously counterproductive. Here, it is rather a homeopathic treatment / dosage. The difference between a poisoning treatment and a treatment that stimulates. Only the dose makes the poison. I would add the duration too. -
@LucH said in High-dose thiamine troubleshooting:
@mostlylurking
I agree with your analyze on excess serotonin and 5-HTP (targeting SSRI, thus increasing central nervous system synthesis of serotonin).
SSRI = Selective Serotonin Reuptake Inhibitor.
Saying that, prucalorid is taken, not as a laxative – at the usual dose of 2 mg – but as a stimulus (0.5 mg resolor). The dose is very weak but sufficient for re-educating a lazy gut.
Here we’re trying to find a solution for colonic motility dysfunction. And the solution has not to be found with a laxative. This is not because of a lack of electrolytes, fibbers or exercises. By the way, 30 grams fibbers is needed, with soothed fibbers (progressive).
When suffering from insufficient electrical contractile bowel movements, between 2 meals, we aren’t targeting a problem of transit. The muscle contractions are called peristalsis. This process must be re-educated. Of course, the IBS problem (high-amplitude propagating contractions) must be taken into account. First calming down irritation, afterwards stimulation of the stasis.
Note that when I took resolor 0.5 mg, I took it 2 hours before bedtime (3-4 days adaptation period).
A box of 28 tablets cut into two parts = 56 days of treatment (cut with a sharp kitchen knife). No need for a second box.
Once a day for stools wasn’t enough to get rid of excess / unbalanced intestinal bacteria. Some bacteria had nothing to do in the second part of the colon.
The problem in now under control, with the help of diamine oxidase. Too much histamine. (NaturDAO, 1 000 000 units).
Note: The warning concerns the usual employment to a high dosage of 5-HTP and against an excess of serotonin. The excesses are obviously counterproductive. Here, it is rather a homeopathic treatment / dosage. The difference between a poisoning treatment and a treatment that stimulates. Only the dose makes the poison. I would add the duration too.I think that the idea that the "lazy gut" must be "reeducated" is pretty silly. I've been through this problem myself for many years and now I've recovered. I did not "reeducate" my "lazy gut". I recovered by supplementing enough thiamine so that my autonomic nervous system could function normally. "insufficient electrical contractile bowel movements" are insufficient because the autonomic nervous system is not sending the electrical impulses via the vagus nerve needed for peristalsis to happen. It's a communication problem between the brain and the intestine via the vagus nerve.
Kindly read the articles that I posted earlier.
If you want to improve transit time, Ray Peat liked to recommend cascara sagrada.
Cascara, energy, cancer and the FDA's laxative abuse
"If someone thinks of constipation as the result of a lack of neuromuscular stimulation, then it might seem reasonable to design a drug that intensifies the contractions produced by one of the natural transmitter substances, such as serotonin, histamine, or acetylcholine. That’s apparently what Novartis did, with tegaserod, a drug that increases the bowel’s sensitivity to serotonin. That drug, called Zelnorm, was approved by the FDA in 2002, after a couple of years of publications praising it. At the time of its approval, there was already evidence that people using it were more likely to have abdominal surgery, especially for gallbladder disease, and there was doubt about its effectiveness." -
@mostlylurking said in High-dose thiamine troubleshooting:
by supplementing enough thiamine so that my autonomic nervous system could function normally. "insufficient electrical contractile bowel movements" are insufficient because the autonomic nervous system is not sending the electrical impulses via the vagus nerve needed for peristalsis to happen. It's a communication problem between the brain and the intestine via the vagus nerve.
The reasoning is good. Thanks for developing.
Could you give details about your "protocol". The posology of thiamin: posology and duration, please. It could help other readers too. + interaction with B2, I suppose.
I had to stop high dose thiamin because of histamine.
Next post for details to come, after your answer, to avoid interference
Thanks for comprehension.B1 / Thiamine Causing Histamine Issues
-
@LucH said in High-dose thiamine troubleshooting:
@mostlylurking said in High-dose thiamine troubleshooting:
by supplementing enough thiamine so that my autonomic nervous system could function normally. "insufficient electrical contractile bowel movements" are insufficient because the autonomic nervous system is not sending the electrical impulses via the vagus nerve needed for peristalsis to happen. It's a communication problem between the brain and the intestine via the vagus nerve.
The reasoning is good. Thanks for developing.
Could you give details about your "protocol".I follow Dr. Costantini's protocol for thiamine hcl dosage amounts. The amount is based on body weight. I take 1 gram of thiamine hcl mid morning and 1 gram of thiamine hcl mid afternoon. I also take 100mg riboflavin + 100mg niacinamide 4Xday. I take 3100mg of magnesium glycinate divided into 2 doses/day(=400mg pure magnesium). I also take a little biotin, a little b5, a little b6, some k2, some D3, some pregnenolone, some progesterone, some ground eggshells, some selenium, a little NAC, and some zinc daily. I'm relying on orange juice and bananas for my potassium for now; I'm considering trying some potassium bicarbonate though.
High dose thiamine is believed to use up riboflavin, potassium, zinc; I take the other things after reading about them in Ray Peat's written articles.
The posology of thiamin: posology and duration, please. It could help other readers too. + interaction with B2, I suppose.
I rely on the knowledge of Dr. Costantini for dosage (see link above). I'm taking this amount of thiamine hcl for the foreseeable future; I have mercury toxicity with causes high oxidative stress which uses up thiamine. Mercury is extremely toxic and cannot be safely chelated out of the body with currently available protocol.
I consider my vitamin protocol to be a continuing project, due to my heavy metal toxicity; the protocol is not going to "cure" me because the mercury is not going away. Although thiamine is believed to chelate heavy metals (like lead), I think it would not be wise for me to assume that it chelates mercury. Mercury has high affinity for selenium and good results have been seen using selenium+NAC (makes selenocysteine) to resolve mercury in early exposure. My issue is chronic as the exposure happened from childhood amalgams + amalgam removal with zero safety protocols when I was in my 20's; I'm 74 now. I am hypothyroid and am being successfully treated by an elderly endocrinologist with an optimized dose of prescription NP Thyroid by Acella.
Here is an article about the use of thiamine + riboflavin:
Thiamine and Riboflavin for Chronic Fatigue I was diagnosed with CFS around 2000 and suffered from those symptoms for around 30 years. I no longer have those symptoms.Elliot Overton has mentioned that high dose thiamine can use up riboflavin. I think it was in a video, but I don't remember which one. I'm pretty sure it was one of these.
You might find these videos with Elliot of interest:
The Art & Science of Mega-Dose Thiamine Lecture: Part 1
How to Apply High-Dose Thiamine Protocols in Clinical Practice: Part 2I had to stop high dose thiamin because of histamine.
Next post for details to come, after your answer, to avoid interference
Thanks for comprehension.B1 / Thiamine Causing Histamine Issues
Although I lived through decades of strong histamine reaction caused by an immune system run amuck with almost universal reaction to foods and environmental toxins, I no longer have those symptoms. I attribute my recovery to resolving high estrogen via progesterone plus my high thiamine hcl protocol. You can search for "histamine and estrogen" for further reading. Here's an article that touches on the immune system and thiamine.
This Ray Peat article may be helpful:
Serotonin, depression, and aggression: The problem of brain energy
"Serotonin and estrogen have many systematically interrelated functions, and women are much more likely to suffer from depression than men are. Serotonin and histamine are increased by estrogen, and their activation mimics the effects of estrogen. Serotonin is closely involved in mood disorders, but also in a great variety of other problems that affect women much more frequently than men. These are probably primarily energy disorders, relating to cellular respiration and thyroid function. Liver disease and brain disease, e.g., Alzheimer’s disease, are both much more common in women than in men, and serotonin and estrogen strongly affect the energetic processes in these organs. Liver disease can increase the brain’s exposure to serotonin, ammonia, and histamine. It isn’t just a coincidence that these three amines occur together and are neurotoxic; they are all stress-related substances, with natural roles in signaling and regulation."Here is a list of articles found by searching for "histamine" on hormonesmatter.com.
-
@mostlylurking
Thanks for developing. I appreciate.
I'm going to read further (links) and come back soon after when digested.
See you later.
Correcting Mast Cell Activation Syndrome - Histamine Intolerance - Mastocytosis - Biologix Center for Optimum Health
https://biologixcenter.com/allergies/correcting-mast-cell-activation-syndrome-histamine-intolerance-mastocytosis/
This group does extensive research on histamine and is quite reputable. They list Thiamine/B1 as being a liberator and DAO blocker with certain types of administration:
HIT > Therapy > Medicaments
https://www.histaminintoleranz.ch/en/therapy_medicaments.html#antihistamines
*1 => Thiamin as histamin liberator and DAO inhibitor
Sattler 1985 (PDF with reference on histamine active substance)
Sattler J, Hesterberg R, Lorenz W, Schmidt U, Crombach M, Stahlknecht CD.: "Inhibition of human and canine diamine oxidase by drugs used in an intensive care unit: relevance for clinical side effects?" Agents Actions. 1985 Apr;16(3-4):91-4.
https://pubmed.ncbi.nlm.nih.gov/3925736
(Liste unverträglicher Medikamente (DAO-Hemmer))
Büttiker (same PDF with reference on histamine active substance)
*) Lack of magnesium
Specific change of histamine metabolism in acute magnesium-deficient young rats. - PubMed - NCBI
*1 ## Incompatible medicaments
Histamine liberators
Many agents in medicaments (active substances as well as additives) have the negative effect that they cause mast cell degranulation which leads to release of histamine and other mast cell mediators. They have to be avoided where ever possible according to the agreement with your physician.
DAO-Inhibitors
Many agents in medicaments have the negative effect that they are diamine oxidase inhibitors or inhibitors of other histamine degrading enzymes. They have to be avoided where ever possible according to the agreement with your physician.
List of incompatible active substances in medicaments
This list needs to be completed. Please let us know your experiences with other substances.
Set in excerpt (LucH): Acetyl-cysteine (NAC), aspirin, many barbiturates, bile acid, codeine, gelatin (bone broth), NSAID, quinine, thiamin and tyramine. -
@LucH suggested reading: Reversing Mast Cell Activation and Histamine Intolerance Summit
-
Hi,
I said I would come back and give a comment. I did some research and compile what I’ve understood, so far. An input would be appreciated, if you feel so and have time to deal with. Too many people struggle with so-called auto-immune pathologies when we don’t understood the etiology entirely. Partly true but …
This information could give an alternative, possibly the opportunity to perceive an improvement, if the tissues are not too destroyed. We won’t recuperate the lost synapses but as we only use 10 % of our brain, we are able to bypass and create new connections.Anti-Stress & Neuro-Protective Effects of Thiamine (B1)
Mitochondrial Energy Uploaded thanks to Optimized Enzyme Communication
Key points
• Thiamine (B1) has also neuro-protective effects: Brain & Digestive System.
• B1 must be seen as the fuel for a power plant the bioavailability of which is dependent on enzyme functionality.
• Oxidative and chronic low-grade inflammation induce a metabolic block.
• When giving supra-physiological doses of thiamin to the cells, enzymes come back to normal operating state.
• Universal anti-stress properties of thiamine.
• Impact on mitochondrial respiration: link with ATP production.
• The role of thiamine insufficiency in lower brain dysfunction.
• Connection between the brain, the digestive system and the vagus nerve: Dysautonomia and adaptation to the stress environment when fuel is re-loaded.
• Understanding nutritional deficiencies & functional insufficiencies / dependencies.
Cases reports on pathologies: Energy, SIBO, diabetes, fibromyalgia, Parkinson’s, CVD, thyroiditis, multiple sclerosis, etc.Full post on this link, with explanations, figures, studies links and case reports if you want details and see how to manage in practice.
https://mirzoune-ciboulette.forumactif.org/t2045-english-corner-anti-stress-neuro-protective-effects-of-thiamine-b1#29712 -
Remind: 3 pillars of thiamine repletion
- Identify which vitamin B1 your body needs / is accepted by your metabolism (transport capacity, genetic deficiency).
- At least these cofactors are needed: magnesium, potassium and sodium (in proportions, for the two last ones).
- Some vitamins handles as B-vitamin cofactors. Interaction with other B-vitamins.
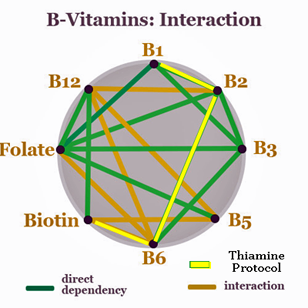
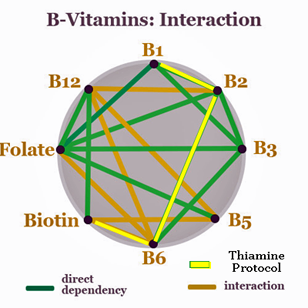
Figure: circle with Vitamins B interaction (B1 B2 B6 Biotin, underlined in yellow)
-
@LucH said in High-dose thiamine troubleshooting:
Hi,
I said I would come back and give a comment. I did some research and compile what I’ve understood, so far. An input would be appreciated, if you feel so and have time to deal with. Too many people struggle with so-called auto-immune pathologies when we don’t understood the etiology entirely. Partly true but …I was diagnosed with rheumatoid arthritis in 2014, the result (I believe) from severely blocked oxidative metabolism caused by hypothyroidism + thiamine deficiency. I recovered via optimized prescription desiccated thyroid medication + some thiamine.
I think that the "auto-immune pathologies" are the result of blocked oxidative energy. I think unblocking/optimizing oxidative energy is curative. If the body has the needed cellular energy, it can heal itself.
This information could give an alternative, possibly the opportunity to perceive an improvement, if the tissues are not too destroyed. We won’t recuperate the lost synapses but as we only use 10 % of our brain, we are able to bypass and create new connections.
Yes. I experienced my brain rewiring itself 1995-1997 after organo-phosphate insecticide poisoning in 1993. Learning a new creative skill that required right brain function facilitated the healing/rewiring.
Anti-Stress & Neuro-Protective Effects of Thiamine (B1)
Mitochondrial Energy Uploaded thanks to Optimized Enzyme Communication
Key points
• Thiamine (B1) has also neuro-protective effects: Brain & Digestive System.Yes. I think that the optimized cellular energy level that thiamine facilitates when working as a co-factor for several enzymes in the Krebs cycle restores the body's balance on the cellular level. Getting the body's energy level working on the cellular level as it is intended is neuro-protective. Think of it as restoring the electrical current that connects the body's cells so that they work in harmony.
• B1 must be seen as the fuel for a power plant the bioavailability of which is dependent on enzyme functionality.
I think it is more accurate to view B1 as a facilitator that allows the fuel (glucose+oxygen) to burn optimally. Dr. Lonsdale's explanation that thiamine acts like a spark plug is a helpful concept.
• Oxidative and chronic low-grade inflammation induce a metabolic block.
The blockage of oxidative metabolism on the cellular level causes inflammation (lactic acidosis). First comes the malfunctioning of the oxidative metabolism (due to thiamine deficiency/functional blockage), which results in an inefficient fuel burn with the end product being lactic acid instead of carbon dioxide. The lactic acid is highly inflammatory. However, it's a double edged sword because high oxidative stress from a poison/irritant like heavy metals deplete thiamine which results in high inflammation.
• When giving supra-physiological doses of thiamin to the cells, enzymes come back to normal operating state.
Yes. Flooding the system with thiamine gets the enzymes to work properly even if there is a weak affinity between enzyme and thiamine. See this video by Elliot Overton.
• Universal anti-stress properties of thiamine.
Yes. I believe thiamine resolves oxidative stress. I think that if you suffer from high oxidative stress (as I have via mercury poisoning) that you will deplete thiamine stores and will benefit from high dose thiamine which will resolve the oxidative stress. See this article: The importance of thiamine (vitamin B1) in humans (search for Oxidative Stress in the article). also see this article: The impact of oxidative stress in thiamine deficiency: A multifactorial targeting issue
• Impact on mitochondrial respiration: link with ATP production.
Yes. Thiamine is required as an enzyme co-factor in oxidative metabolism to make ATP.
• The role of thiamine insufficiency in lower brain dysfunction.
Yes. The lower brain is extremely sensitive to thiamine deficiency which results in problems with the autonomic nervous system. This autonomic nervous system concept encompasses a LOT of things. For example, I suffered for decades from scoliosis (curvature of the spine) because the electrical impulses that controlled the muscles on either side of my spine were not equal in power. I recovered via high dose thiamine hcl. See this article: What Is Scoliosis?
• Connection between the brain, the digestive system and the vagus nerve: Dysautonomia and adaptation to the stress environment when fuel is re-loaded.
Thiamine restores the function of the vagus nerve and resolves dysautonomia. The autonomic nervous system needs the electrical connectivity that oxidative metabolism provides via ATP production. No ATP, no electrical connectivity = dysautonomia.
• Understanding nutritional deficiencies & functional insufficiencies / dependencies.
Cases reports on pathologies: Energy, SIBO, diabetes, fibromyalgia, Parkinson’s, CVD, thyroiditis, multiple sclerosis, etc.Full post on this link, with explanations, figures, studies links and case reports if you want details and see how to manage in practice.
https://mirzoune-ciboulette.forumactif.org/t2045-english-corner-anti-stress-neuro-protective-effects-of-thiamine-b1#29712Good write up, lots of info. Helpful link!
-
@LucH said in High-dose thiamine troubleshooting:
Remind: 3 pillars of thiamine repletion
- Identify which vitamin B1 your body needs / is accepted by your metabolism (transport capacity, genetic deficiency).
Yes, it is important to learn which thiamine would work best for you. For example, some people do very well on TTFD thiamine because it is supposed to get into the body easier and the cells easier than some other kinds. However, if you have poor glutathione status, which can happen if you have high oxidative stress, you will probably react badly to TTFD because it uses glutathione in its chemical function. I had this problem myself and so I take high dose thiamine hcl instead which works well for me.
- At least these cofactors are needed: magnesium, potassium and sodium (in proportions, for the two last ones).
- Some vitamins handles as B-vitamin cofactors. Interaction with other B-vitamins.
I think that it is helpful to understand that if you massively improve the basic function of creating ATP via oxidative metabolism, whether it's from taking thyroid supplement or thiamine supplement or both, the other necessary vitamins and trace minerals are going to get used more too, simply because the factory is back up and running. This can cause other deficiencies so it is helpful to research to learn which nutrients might be most susceptible to deficiency. For me these include: niacinamide, riboflavin, biotin, magnesium, potassium, selenium, zinc.
Blood testing is a really good idea because this can get complicated and confusing. Also keep in mind that too much thyroid supplement can result in hyperthyroidism which can cause a thiamine deficiency which results in symptoms identical to hypothyroidism so blood testing is needed to determine what is really going on.
Figure: circle with Vitamins B interaction (B1 B2 B6 Biotin, underlined in yellow)
-
@Mostlylurking
Thanks for your input. I really appreciate the comments. It emphasizes very well the efficacy / the value of HDT (high physiological dose).
I’d like to put this point into excerpt:
*) Why to give HDT?When giving supra-physiological doses of thiamin to the cells, enzymes come back to normal operating state. (1)
=> We aim to increase the exchange through passive and active ways. The active way is made through enzyme transporters. The passive way is through cell membranes, if there aren’t too many blockers (from oxidative stress and chronic low-grade inflammation e.g.).
We know that the traditional way of transport of B1 TPP (from food) is through gastrointestinal phosphatases, before reaching blood flood. This B1 was thought to be only a water-soluble vitamin. It’s not. TPP can also be transported across cell membranes (2) but likely less well absorbed than benfotiamine or TTFD.
TPP = thiamine pyrophosphate.
*) Why and when nutritional intake is not sufficient.
If we read the conventional recommendations from authorities there is only a problem for 6% of the US population. (3) That’s what the blood tests mention. Right but what about your optimal energy level or your brain functioning? See here the difference of appreciation: an impaired metabolism with a metabolic disorder of thyroid or glycemia if left untreated (not perceived before it’s too late because the Gauss’s curve has said so). Traditional medicine sees the failure but doesn’t always / usually anticipate the problems from slow carburation. That’s just one example.
Gauss’s curve
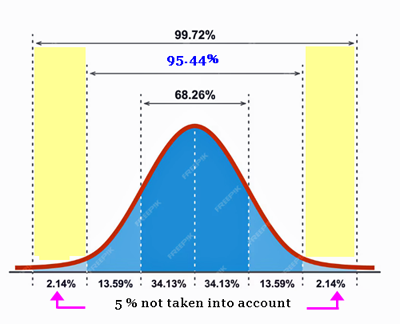
The Gauss's curve analogy here emphasizes the concept of the "tail end" of the curve, where about 5% of cases fall outside the normal range. In this context, it suggests that there's a small percentage of cases where the metabolic disorder isn't perceived until it's too late. ## Traditional medicine tends to focus on the majority of cases within the normal range and may overlook or underestimate the significance of these outliers.
So, while traditional medicine might not see a problem because the majority of cases appear normal, it fails to anticipate the issues that arise from the small percentage of cases where metabolic disorders aren't detected early. This leads to the problem being left untreated, as it's not recognized until it's already advanced.
In summary, the Gauss's curve illustrates how the small percentage of cases falling outside the normal range can be overlooked, leading to the problem being untreated until it reaches a critical stage.
Metabolic Block
Are you exposed to “stress” factors that block your assimilation for the brain? As already seen, “thiamine (vitamin B1) is critical for the metabolism of food into cellular energy or ATP. Without sufficient thiamine, cellular energy wanes, and with it, the capacity to maintain the energy to function declines. Chronic, unrelenting fatigue is a common characteristic of insufficient thiamine. At its root, fatigue is the physical manifestation of poor energy metabolism”. (4)Your appropriate blood test is then not going to explain anything.
Here are some case reports mentioning the insufficiency of the DRI (Daily Recommended Intake).
Diabetes
The proportion of people with type 1 or type 2 diabetes who have poor thiamin status based on erythrocyte transketolase activity ranges from 17% to 79% in studies conducted to date [40]. In a study of 76 consecutive patients with type 1 or type 2 diabetes, for example, 8% had mild thiamin deficiency and 32% had moderate deficiency based on assays of the transketolase enzyme [33].
Heart failures
The rates of poor thiamin status in patients with heart failure have ranged in studies from 21% to 98% [47]. Explanations for this association include older age, comorbidities, insufficient dietary intake, treatment with diuretics, and frequent hospitalizations [48].
The authors of one study reported that 33% of 100 patients with chronic heart failure had thiamin deficiency compared to 12% of 50 healthy volunteers [49]. Rates of deficiency were even higher when the investigators excluded those who used thiamin supplements.
Alzheimer’s disease
Thiamin deficiency produces oxidative stress in neurons, death of neurons, loss of memory, plaque formation, and changes in glucose metabolism—all markers of Alzheimer’s disease. Autopsy studies have shown that transketolase and other thiamin-dependent enzymes have decreased activity in the brains of people with Alzheimer’s disease [52,53].
Few studies have assessed the prevalence of thiamin deficiency in people with Alzheimer’s disease. One of these studies found that 13% of 150 patients with cognitive impairment and acute-onset behavioral disturbances were considered thiamin deficient based on plasma levels [26].
Note: Analysis based on plasma level gives only indication on short term. And not what is burned or blocked further in the process of assimilation.
Maintenance and Performance of the Brain
As already seen, thiamine plays a key role in the maintenance of brain function: Thiamine diphosphate is a cofactor for several enzymes involved in glucose metabolism whereas thiamine triphosphate has distinct properties at the neuronal membrane. (5) We need different forms of B1 to optimize different functions, and particularly to reach effects onto mitochondrial respiration.
Sources and References- Elliot Overton
- How is B1 from food assimilated?
DOI: 10.1534/genetics.104.028605
Dietary thiamine (vitamin B1) consists mainly of thiamine pyrophosphate (TPP), which is transformed into thiamine by gastrointestinal phosphatases before absorption. It was believed that TPP itself cannot be transported across plasma membranes in significant amounts, which forms TPP from thiamine at the expense of ATP inside cells. (…) These observations indicate that, in contrast to expectation from previous evidence, TPP can be transported across cell membranes. We also find that thiamine supplementation partially rescues the phenotype of partial loss-of-function mutants of the Na/K ATPase, providing genetic evidence that thiamine absorption, and/or redistribution from the absorbing cells, requires the full activity of this enzyme.
=> Comment Luch: We need the transketolase enzyme to absorb well this type of B1 (TPP from food). To fully absorb the benefits of TPP, passive transport through membranes is required. - The average daily thiamin intake from foods and supplements in adults age 20 and older is 4.89 mg. An analysis of data from the 2003–2006 National Health and Nutrition Examination Survey showed that only 6% of the U.S. population has a usual intake below the EAR.
https://ods.od.nih.gov/factsheets/Thiamin-HealthProfessional/#h6
The World Health Organization recommends daily oral doses of 10 mg thiamin for a week, followed by 3–5 mg/daily for at least 6 weeks, to treat mild thiamin deficiency. - Dr. Chandler Marrs talking about Thiamin. April 2022
Introduction to a video, talking with Scott Scott Forsgren, FDN-P.
https://www.hormonesmatter.com/talking-about-thiamine/ - Thiamine diphosphate is a cofactor for several enzymes involved in glucose metabolism whereas thiamine triphosphate has distinct properties at the neuronal membrane
https://mirzoune-ciboulette.forumactif.org/t2045-english-corner-anti-stress-neuro-protective-effects-of-thiamine-b1#29713
-
@LucH said in High-dose thiamine troubleshooting:
@Mostlylurking
Thanks for your input. I really appreciate the comments. It emphasizes very well the efficacy / the value of HDT (high physiological dose).
I’d like to put this point into excerpt:
*) Why to give HDT?When giving supra-physiological doses of thiamin to the cells, enzymes come back to normal operating state. (1)
=> We aim to increase the exchange through passive and active ways. The active way is made through enzyme transporters. The passive way is through cell membranes, if there aren’t too many blockers (from oxidative stress and chronic low-grade inflammation e.g.).
Well, this certainly is a gigantic caveat, isn't it? If ANYTHING disrupts oxidative metabolism, inflammation goes way up due to lactic acid increase. Any oxidative stress (from toxins like heavy metals, etc.) depletes thiamine which throws a ringer into oxidative metabolism.
We know that the traditional way of transport of B1 TPP (from food) is through gastrointestinal phosphatases, before reaching blood flood. This B1 was thought to be only a water-soluble vitamin. It’s not. TPP can also be transported across cell membranes (2) but likely less well absorbed than benfotiamine or TTFD.
TPP = thiamine pyrophosphate.
*) Why and when nutritional intake is not sufficient.There's some research in the salmon fishing industry that you might find very interesting. When the salmon are exposed to more PUFA in their diet in relationship to thiamine availability their health suffers and the low ratio of thiamine to PUFA can cause the fry (baby salmon) hatch to die. The solution for the problem is to put thiamine in the water. links:
https://hmr.biomedcentral.com/articles/10.1186/s10152-020-00542-9https://www.mdpi.com/2410-3888/9/2/58
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6182616/
There seems to be better research for the salmon fishing industry than there is for human health.
If we read the conventional recommendations from authorities there is only a problem for 6% of the US population.
I suspect that the authorities came to that deduction via the WAG method.
(3) That’s what the blood tests mention. Right but what about your optimal energy level or your brain functioning? See here the difference of appreciation: an impaired metabolism with a metabolic disorder of thyroid or glycemia if left untreated (not perceived before it’s too late because the Gauss’s curve has said so). Traditional medicine sees the failure but doesn’t always / usually anticipate the problems from slow carburation. That’s just one example.
You are overly generous re. the abilities of traditional medicine. I'm much more of a cynic due to my own personal experiences with doctors. I agree; what about optimal oxidative metabolism and brain function? The health industry is beyond broken.
Gauss’s curve
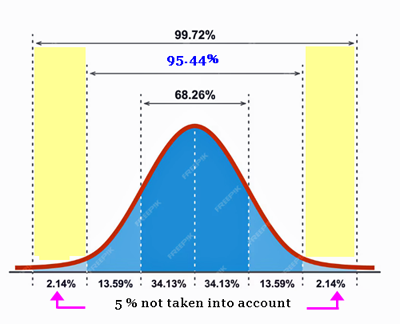
The Gauss's curve analogy here emphasizes the concept of the "tail end" of the curve, where about 5% of cases fall outside the normal range. In this context, it suggests that there's a small percentage of cases where the metabolic disorder isn't perceived until it's too late. ## Traditional medicine tends to focus on the majority of cases within the normal range and may overlook or underestimate the significance of these outliers.
So, while traditional medicine might not see a problem because the majority of cases appear normal, it fails to anticipate the issues that arise from the small percentage of cases where metabolic disorders aren't detected early. This leads to the problem being left untreated, as it's not recognized until it's already advanced.My own experience has been that traditional medicine doesn't see the problem because they have not bothered to look. Most medical doctors are clueless when it comes to things like the Krebs cycle and what might go wrong. They are trained to prescribe pharmaceutical drugs; they get no education regarding vitamins/minerals.
In summary, the Gauss's curve illustrates how the small percentage of cases falling outside the normal range can be overlooked, leading to the problem being untreated until it reaches a critical stage.
If you happen to be on the far side of 60, you are more likely to be thiamine deficient because the gut tends to lose its ability to absorb thiamine. But doctors will take one look at your age and write off your symptoms as being caused by "aging".
Happily, thiamine is considered a safe supplement and the easiest way to test to see if you would benefit from supplementing it is to take some. Researching online is a good idea.
suggested videos:
Vitamin B1 Deficiency - Pharma Harma (it's short)
and
The Ultimate Crash Course on Vitamin B1 - Fatigue, Nerve Pain, Heart Disease & More (it's long but very good!)Metabolic Block
Are you exposed to “stress” factors that block your assimilation for the brain? As already seen, “thiamine (vitamin B1) is critical for the metabolism of food into cellular energy or ATP. Without sufficient thiamine, cellular energy wanes, and with it, the capacity to maintain the energy to function declines. Chronic, unrelenting fatigue is a common characteristic of insufficient thiamine. At its root, fatigue is the physical manifestation of poor energy metabolism”. (4)Your appropriate blood test is then not going to explain anything.
Here are some case reports mentioning the insufficiency of the DRI (Daily Recommended Intake).
Diabetes
The proportion of people with type 1 or type 2 diabetes who have poor thiamin status based on erythrocyte transketolase activity ranges from 17% to 79% in studies conducted to date [40]. In a study of 76 consecutive patients with type 1 or type 2 diabetes, for example, 8% had mild thiamin deficiency and 32% had moderate deficiency based on assays of the transketolase enzyme [33].
Heart failures
The rates of poor thiamin status in patients with heart failure have ranged in studies from 21% to 98% [47]. Explanations for this association include older age, comorbidities, insufficient dietary intake, treatment with diuretics, and frequent hospitalizations [48].
The authors of one study reported that 33% of 100 patients with chronic heart failure had thiamin deficiency compared to 12% of 50 healthy volunteers [49]. Rates of deficiency were even higher when the investigators excluded those who used thiamin supplements.
Alzheimer’s disease
Thiamin deficiency produces oxidative stress in neurons, death of neurons, loss of memory, plaque formation, and changes in glucose metabolism—all markers of Alzheimer’s disease. Autopsy studies have shown that transketolase and other thiamin-dependent enzymes have decreased activity in the brains of people with Alzheimer’s disease [52,53].
Few studies have assessed the prevalence of thiamin deficiency in people with Alzheimer’s disease. One of these studies found that 13% of 150 patients with cognitive impairment and acute-onset behavioral disturbances were considered thiamin deficient based on plasma levels [26].
Note: Analysis based on plasma level gives only indication on short term. And not what is burned or blocked further in the process of assimilation.
Maintenance and Performance of the Brain
As already seen, thiamine plays a key role in the maintenance of brain function: Thiamine diphosphate is a cofactor for several enzymes involved in glucose metabolism whereas thiamine triphosphate has distinct properties at the neuronal membrane. (5) We need different forms of B1 to optimize different functions, and particularly to reach effects onto mitochondrial respiration.I think what we really need is for doctors to understand how common thiamine deficiency/functional blockage actually is and the damage/symptoms it causes. They do not find what they are not testing for. They are led to believe that possible thiamine deficiency was resolved decades ago via the addition of thiamine to refined grain products.
Sources and References
- Elliot Overton
- How is B1 from food assimilated?
DOI: 10.1534/genetics.104.028605
Dietary thiamine (vitamin B1) consists mainly of thiamine pyrophosphate (TPP), which is transformed into thiamine by gastrointestinal phosphatases before absorption. It was believed that TPP itself cannot be transported across plasma membranes in significant amounts, which forms TPP from thiamine at the expense of ATP inside cells. (…) These observations indicate that, in contrast to expectation from previous evidence, TPP can be transported across cell membranes. We also find that thiamine supplementation partially rescues the phenotype of partial loss-of-function mutants of the Na/K ATPase, providing genetic evidence that thiamine absorption, and/or redistribution from the absorbing cells, requires the full activity of this enzyme.
=> Comment Luch: We need the transketolase enzyme to absorb well this type of B1 (TPP from food). To fully absorb the benefits of TPP, passive transport through membranes is required. - The average daily thiamin intake from foods and supplements in adults age 20 and older is 4.89 mg. An analysis of data from the 2003–2006 National Health and Nutrition Examination Survey showed that only 6% of the U.S. population has a usual intake below the EAR.
Oh, dear.... I wonder if they took into account the population's intake of PUFA (see the salmon studies above).
https://ods.od.nih.gov/factsheets/Thiamin-HealthProfessional/#h6
The World Health Organization recommends daily oral doses of 10 mg thiamin for a week, followed by 3–5 mg/daily for at least 6 weeks, to treat mild thiamin deficiency.The WHO? That organization that is focused on population reduction? They call it "sustainable development" I think. It's part of Agenda 2030.
- Dr. Chandler Marrs talking about Thiamin. April 2022
Introduction to a video, talking with Scott Scott Forsgren, FDN-P.
https://www.hormonesmatter.com/talking-about-thiamine/ - Thiamine diphosphate is a cofactor for several enzymes involved in glucose metabolism whereas thiamine triphosphate has distinct properties at the neuronal membrane
https://mirzoune-ciboulette.forumactif.org/t2045-english-corner-anti-stress-neuro-protective-effects-of-thiamine-b1#29713