Conditional problems with vitamin A: a place for sane discussions
-
On retinaldehyde metabolism
Molecular weights:
- Glucose: 180 g per 1 mol
- Glyceral(dehyde): 90 g per 1 mol
- Retinol: 290 g per 1 mol (290 μg per 1 μmol)
A person may consume 1 mol of glucose (180 g) in a day and complain of issues with retinol while ingesting 1 μmol (290 μg) of it.
Glucose is split at some stage of its oxidation:
- 1 glucose → 2 glyceral(dehyde 3-phosphate)
In the situation above, the body would have to process 2 mol of aldehydes in a day from glucose alone.
Glyceral dehydrogenase and retinal dehydrogenase depend on NAD+ for oxidation.
It's possible that the ratio of NAD+ to NADH affects the metabolism of poisons in disfavor of oxidation, but the body has enough NAD+ to metabolize..
- 2,000,000 μmol of glyceral
Yet not to metabolize..
- 1 μmol of retinal when needed?
Retinal dehydrogenase would have to be way down the priority rank to get its meager share of NAD+ only after other needs are met. It could have evolved strategically this way to function as a 'nutrostat' and become more active to produce (the regulatory) retinoic acids depending on nourishment state.
However, vitamin A is also involved in the induction of genes related to differentiation. It has to be functional in a phase that's marked by anabolism and likely higher levels of NAD(P)H. If its oxidation was heavily dependent on the oxidized:reduced ratio of NAD, it could be a problem.
If retinoic acids are short-lived and the poison A crowd assume to be stuck with retinal because of inability to process it due to NAD+ insufficiency, how would they explain the elevated level in inflammed tissues, found in the conditions that afflict them?
- Retinoic Acid Is Elevated in the Mucosa of Patients With Active Ulcerative Colitis and Displays a Proinflammatory Role by Augmenting IL-17 and IFNγ Production
- Increased Production of Retinoic Acid by Intestinal Macrophages Contributes to Their Inflammatory Phenotype in Patients With Crohn's Disease
Interestingly, it's by impairing the conversion of retinal to retinoic acids that some researchers could get the immunosuppressive effect that the scaremongers seek to recreate with deprivation:
Retinal dehydrogenase can become saturated, but when its capacity is exceeded or when it's inactive, the body can rely on the generic aldehyde oxidase to metabolize retinal and prevent its accumulation, and it doesn't depend on NAD+. Therefore, NAD+ is important, but not essential for the conversion of retinal to retinoic acid.
"Cytosolic enzymes appear to be responsible for the overwhelming majority of atRA formation from at-retinal [28–31]. The ALDH enzymes along with AOX and XOX are cytosolic soluble enzymes that form atRA from at-retinal [32, 33]. While ALDH enzymes are NAD(P)+ dependent, AOX and XOX do not require a pyridine nucleotide cofactor for their activity [17, 33], and the necessity of NAD(P)+ for the majority of atRA formation in the mouse liver was used to show that ALDH enzymes contribute to the majority of atRA formation [30]. An AOX inhibitor, pyridoxal, only inhibited approximately 5% of the atRA formation. Similarly, 80% of the atRA formation in human liver cytosol was NAD+ dependent and the overall contribution of AOX was approximately 10% [31]. Whether microsomal NADPH dependent enzymes such as cytochrome P450s contribute to in vivo atRA synthesis is poorly studied. This is mainly because the Km values for at-retinal with cytochrome P450 are nearly 70-fold higher than endogenous concentrations of at-retinal suggesting they most likely do not have a significant role in atRA biosynthesis [16, 24]. In contrast, the Km values for at-retinal with ALDH1A1-1A3 are low nanomolar [34]. The ALDH1A enzymes also catalyze the formation of atRA from at-retinal bound to cellular retinol binding protein 1 (CRBP1) which is expressed ubiquitously across the body [35–37]."
Aldehyde Oxidase Contributes to All-Trans-Retinoic Acid Biosynthesis in Human Liver
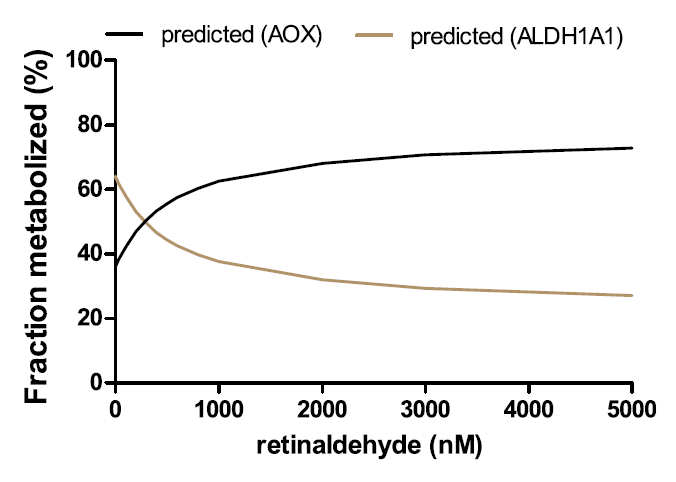
"This study unequivocally shows that AOX forms atRA from retinaldehyde and that in human liver ALDH1A1 and AOX contribute to atRA biosynthesis. Recombinant AOX exhibited about 6-fold higher Km and 1.6-fold higher CLint than ALDH1A1 for atRA formation, showing that ALDH1A1 is a high-affinity, low-capacity atRA synthesizing enzyme, whereas AOX is a low-affinity, high-capacity enzyme. According to the human protein atlas data base, AOX protein is expressed in the kidney, bladder, pancreas, endocrine tissues, and reproductive tissues. This suggests that AOX may contribute to atRA synthesis in the testis, among other tissues. However, studies in healthy mice have shown that AOX activity is not quantitatively significant in the mouse testis (Arnold et al., 2015a) but rather that AOX plays a role in testicular atRA synthesis in mice when ALDH1A activity is impaired (Beedle et al., 2019). This is in agreement with the findings in the human testis showing that ALDH1A1 and ALDH1A2 are responsible for >95% of atRA formation in this tissue (Arnold et al., 2015). In contrast to the testis, AOX appears to contribute about 50% of atRA biosynthesis in mouse liver (Arnold et al., 2015a). This suggests a tissue-specific role of AOX that likely depends on the expression levels of AOX and the complement of ALDH1A enzymes expressed in the different tissues. The results of this study support a similar role of AOX in atRA biosynthesis in human liver as in the mouse liver, with AOX contributing between 33% and 70% of atRA biosynthesis depending on retinaldehyde concentration."
"The reported total concentrations of retinaldehyde in the liver and adipose are 100–200 pmol/g (~150 nM) (Ziouzenkova et al., 2007; Kane et al., 2008). These concentrations are much below the Km toward AOX (1.5 mM) but similar to the Km toward ALDH1A1 (0.25 mM). Because of the difference in Km values for AOX and ALDH1A1, the predicted and observed fm values of retinaldehyde by AOX show a clear dependence on retinaldehyde concentration within the evaluated range of 20–2,000 nM retinaldehyde. As the concentration of retinaldehyde increases, fm,AOX increases due to the saturation of the high-affinity ALDH1A1."
"This also suggests that in the case of ALDH1A dysfunction (inhibition, downregulation, or genetic defect) or excess retinoid/vitamin A (saturation of ALDH1A1), AOX plays an important role in regulating hepatic vitamin A homeostasis. The relative contribution of AOX (30%–70%) to atRA biosynthesis is supported by the scaling of atRA formation from recombinant enzymes, the quantification of AOX and ALDH1A1 protein expression in the liver, the cofactor dependence of atRA formation, and the inhibition of atRA formation by selective ALDH1A and AOX inhibitors WIN18,446 and hydralazine. These tools developed in the current study allow differentiation of ALDH1A and AOX contributions to atRA formation and can be further applied to other critical retinoid responsive tissues, such as the skin, hematopoietic cells, and adipose tissue, to determine the enzymes contributing to atRA biosynthesis. Such information will be useful in predicting how inhibition or genetic variability in AOX and ALDH1A enzymes will affect retinoid homeostasis and signaling."
Two different enzymes are primarily responsible for retinoic acid synthesis in rabbit liver cytosol
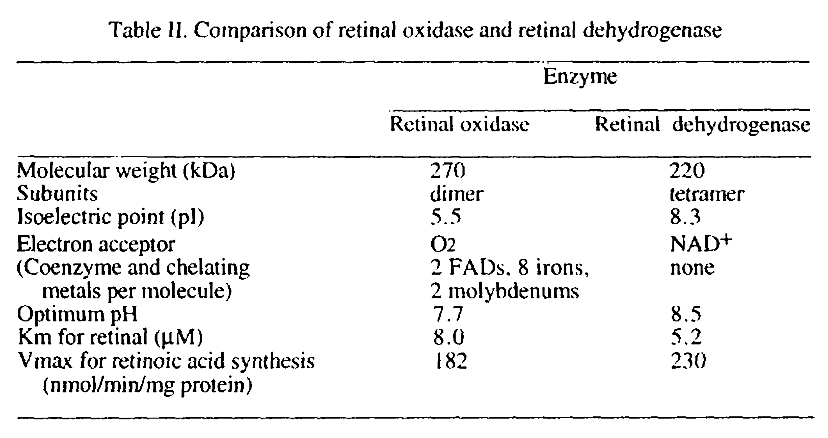
Values aren't reliable.
The preferred route doesn't depend on molybdenum. The alternative route result in formation of hydrogen peroxide, but the amounts shouldn't be monstrous, although it could occur at susceptible sites.
Choline isn't used up in esterifying retinol
If retinal couldn't be oxidized by any means, it could be converted to retinol for temporary storage.
The enzymes involved in esterification are acyltransferases:
- Lecithin:retinol acyltransferase (also high-affinity, low-capacity)
- Acyl-CoA:retinol acyltransferase
Genetic Variations Associated with Vitamin A Status and Vitamin A Bioavailability
"LRAT uses fatty acids from intracellular membrane phospholipids, while DGAT1 and the other ARAT(s) use newly-absorbed fatty acids[.]"
Phosphatidylcholine functions as a fatty acid donor and retinol would be the acceptor (to yield retinyl palmitate, stearate, oleate..). What's being consumed is the fatty acid of a structural lipid, not its choline. After the reaction, the lost fatty acid of phosphatidylcholine can be replenished and the molecule will be renewed.
If a lack of choline is severe enough to compromise cell structure, the person has greater concerns than the esterification of retinol. And the body can switch to the alternative pathway.
Free retinol appears in circulation after meals with higher vitamin A doses, showing that the esterification process can be overwhelmed, but it can be prevented by avoiding equine amounts at once and by consuming extra fat with the meal to cooperate with the backup acyltransferase.
-
Vitamin A increases SCD1 7x. That alone is reason to take it easy
-
Thank you for this. I wonder if i would get banned for posting this in ray peat forum now.
-
@Verdad I doubt it. None of the people left there would even understand half of what A. wrote.
-
@Kvothe He has terrific word play, Calcium = Kilcium, love that Guy

-
@Not_James_Bond we all do
-
You guys should look into the RXR. Its a very interesting nuclear receptor.
-
@Kvothe I would not be surprised he seems to be basically banning anyone who disagrees with him. He sounds like a deranged cult leader i think it will not be long till he bans anyone posting anything that goes against his theories.
Soon it will be if you post a positive study about Vitamin A or calcium it will be a banning ofense.
-
On niacin for NAD
Nicotinamide is now regarded as toxic and nicotinic acid is being favored. It's supplemented intending to increase the synthesis of NAD to detoxify poisons.
They're not using pharmacological amounts of niacin that would lead to marked differences in how each form is eliminated. The moderate doses in use should be readily converted to nicotinamide. This is how forms are metabolized in mice:
The Management of Nicotinamide and Nicotinic Acid in the Mouse
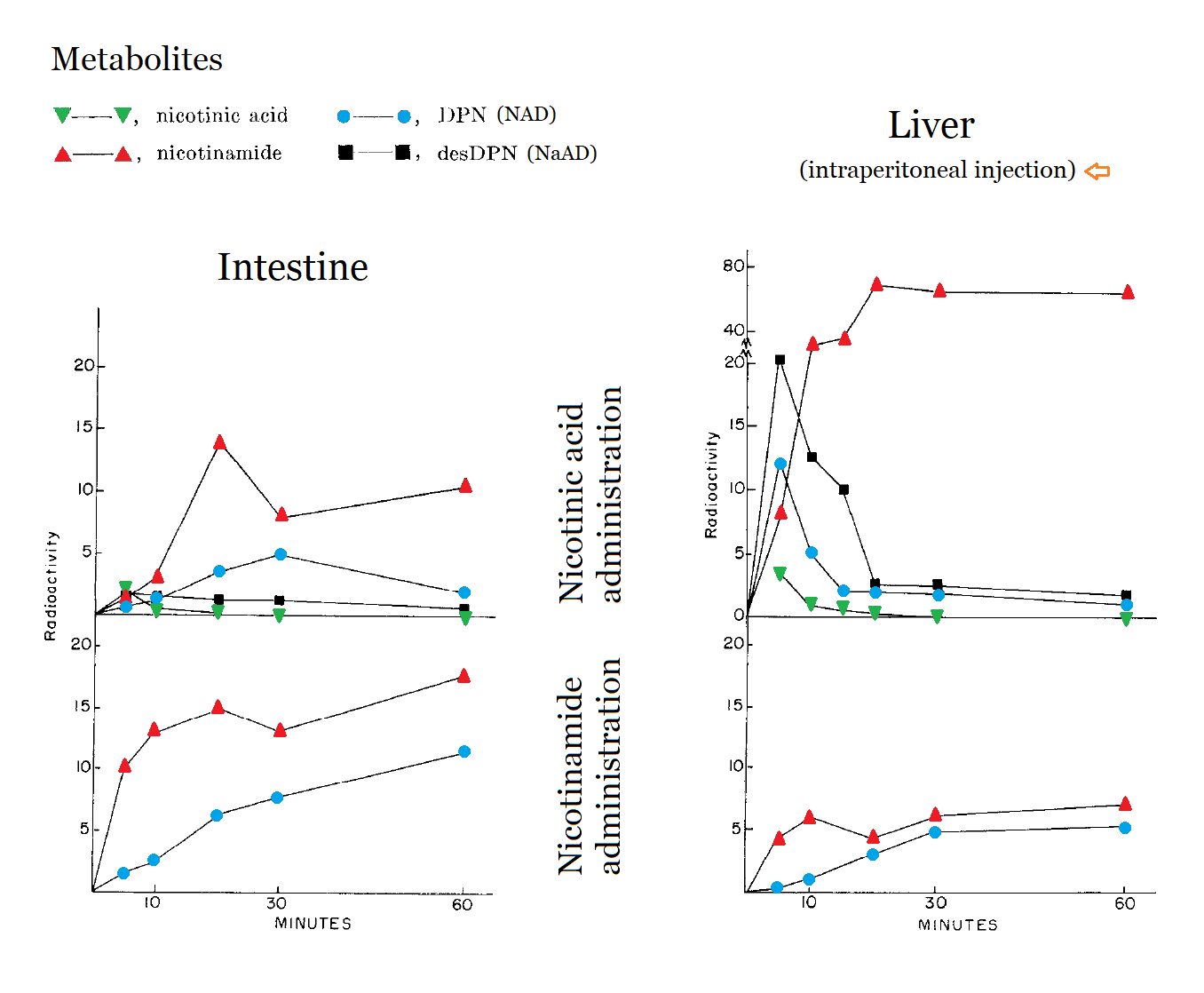
DPN = NAD
desDPN = NaAD (immediate precursor to NAD)
↳ 'des' here stands for 'desamidated' NAD.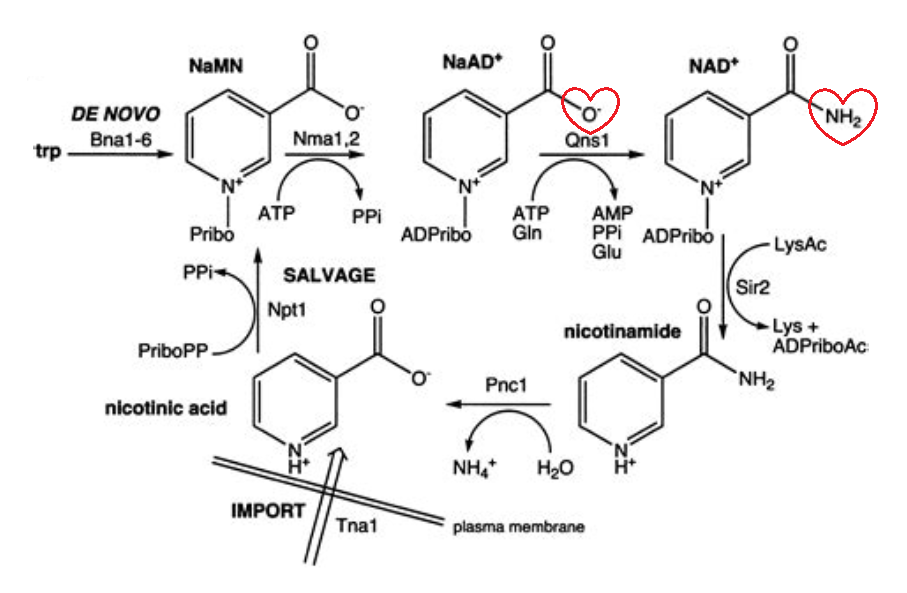
Nicotinamide as yield happens with nicotinamide riboside or mononucleotide too:
"NR and NMN were administered by i.v. bolus or oral gavage at 50 mg/kg, which is equivalent to 290 mg in a 70-kg human on a body surface area basis, in the range of common nutraceuticals."
"Unlike in cell culture, where NR and NMN are readily incorporated into NAD (Ratajczak et al., 2016; Frederick et al., 2016), oral administration fails to deliver NR or NMN to tissues without breaking the nicotinamide-ribose bond."
"Irrespective of the route of delivery, the main circulating product of the administered NR or NMN was NAM, which increased by ~20⨯ within 5 min of i.v. NR or NMN; oral NR or NMN administration led to a more modest rise in circulating NAM (Figure 7C)."
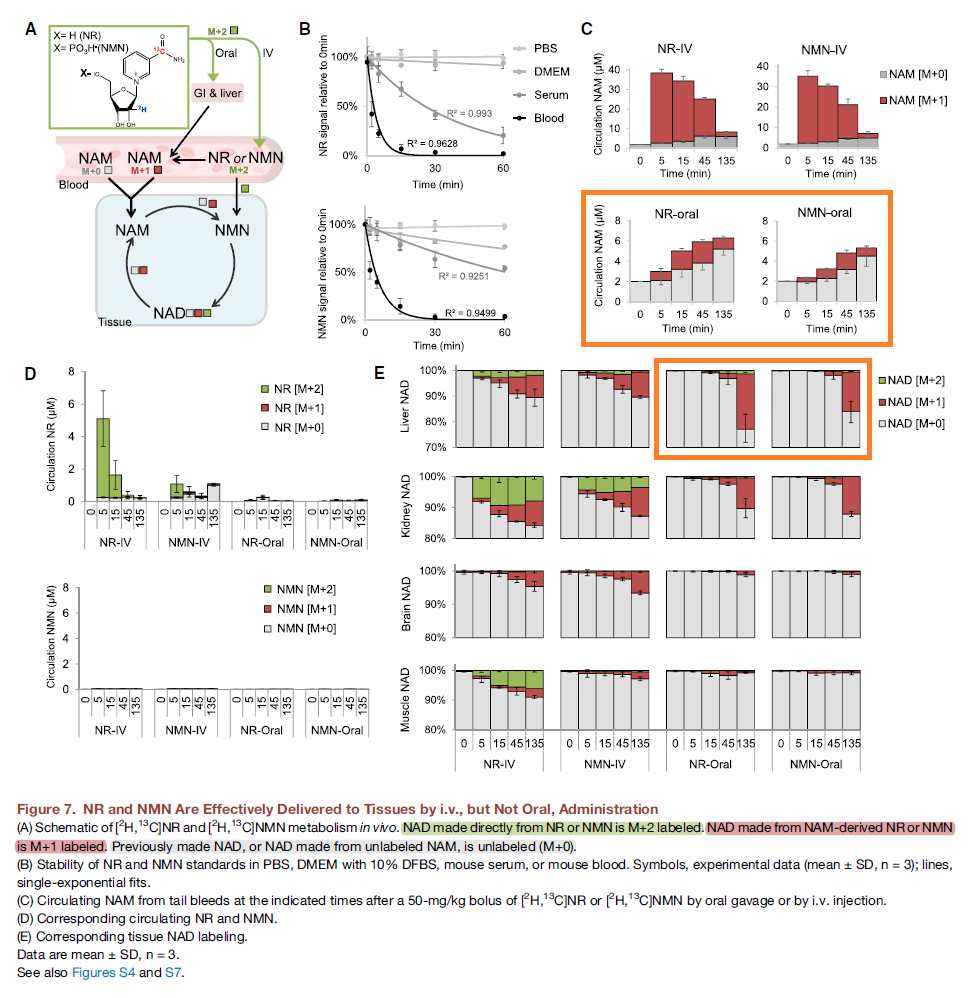
I wonder how they justify their aversion to nicotinamide in moderate doses.
-
@thyroidchor27 said in Conditional problems with vitamin A: a place for sane discussions:
Vitamin A increases SCD1 7x. That alone is reason to take it easy
Retinoic acids levels are kept relatively stable. What are the conditions for it to occur?
Guys, it was member 'schultz' who started the kill- term trend.
-
@Amazoniac in the plasma or in the liver????
-
They pride themselves on the fact that it's possible to put psoriasis into remission through poison A deprivation, but what about Coimbra's experiment who accomplished the same with "vitamin" D3 (875 mcg/d) and minor dietary modifications?
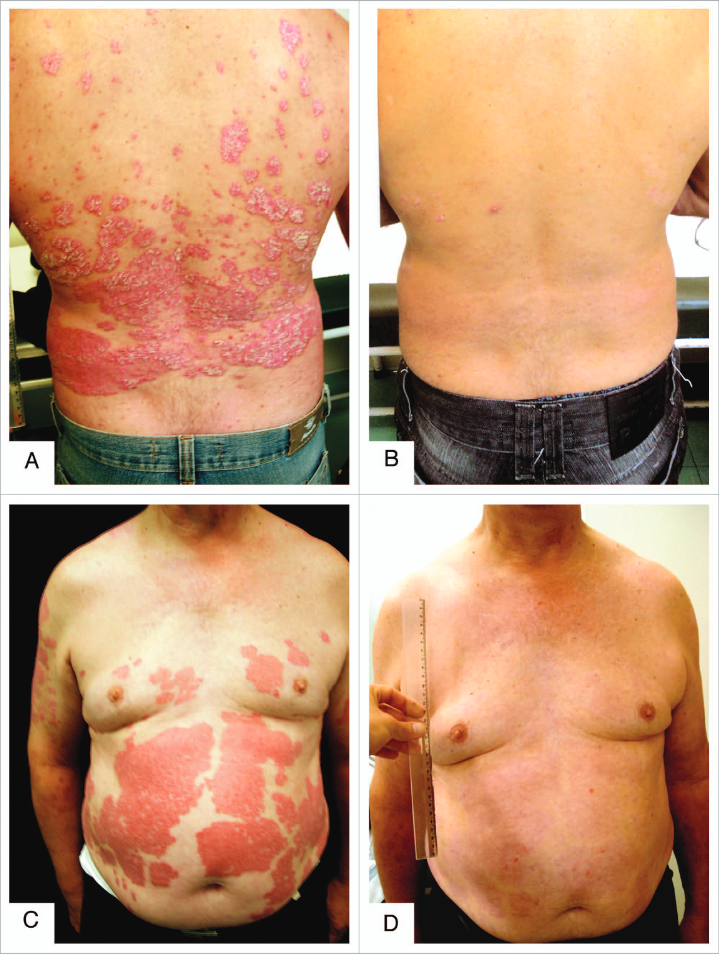
These approaches work, but are rudimentary. They manipulate upstream processes rather favoring targeting downstream specifics, that minimize the risk of having to compromise other functions to reach the therapeutic dose (for low or for high).
Psoriasis and beyond: targeting the IL-17 pathway | Nature
Even though targeting what's downstream is more sophisticated, the best thing to do is to try to address the pathogen above it all.
-
@thyroidchor27 said in Conditional problems with vitamin A: a place for sane discussions:
@Amazoniac in the plasma or in the liver????
That claim is based on what?
-
By the way, you can find various reports of 'undetectable' vitamin D levels; some because of analysis error (it can be challenging to quantify toxins that occur in modest amounts), but others not.
Controlling the availability of the precursor molecule can be a means to make up for an overactive pathway:
Undetectable serum calcidiol: not everything that glitters is gold
"Granulomatous hypercalcaemia is particularly sensitive to vitamin D administration even though toxic 25(OH) vitamin D levels are not reached [5]. This has been attributed to avid 25(OH) vitamin D metabolism into 1,25(OH)2 vitamin D by macrophage 1α-hydroxylase. Availability of 25(OH) vitamin D becomes the main regulator of 1,25(OH)2 vitamin D synthesis. Under these circumstances, treatment of vitamin D deficiency will increase the availability of 25(OH) vitamin D and lead to high 1,25(OH)2 vitamin D levels and hypercalcaemia [8, 9]."
-
@Amazoniac said in Conditional problems with vitamin A: a place for sane discussions:
They pride themselves on the fact that it's possible to put psoriasis into remission through poison A deprivation, but what about Coimbra's experiment who accomplished the same with "vitamin" D3 (875 mcg/d) and minor dietary modifications?
Have they presented any evidence regarding vitamin A deprivation and psiorasis, except tweets from good guy Garret Smith and the bible?
-
@Kvothe, I'm going by trust in the accounts of reliable people.
-
@Amazoniac Are there any in that crowd, and have they controlled their conclusions for other variables? The highly restrictive diets they eat exclude a huge lists of potential irritants that might cause auto-immune conditions and symptoms.
-
@Kvothe said in Conditional problems with vitamin A: a place for sane discussions:
@Amazoniac Are there any in that crowd, and have they controlled their conclusions for other variables? The highly restrictive diets they eat exclude a huge lists of potential irritants that might cause auto-immune conditions and symptoms.
'Maybe' to both questions. However, the accounts would be founded.
The Effect of Restricted Intake of Carotene and Vitamin A on Psoriasis Vulgaris
The exclusion of other toxins can contribute to the remission, but I don't think that the addition of isolated poisons to their current diets would lead to positive outcomes.
-
@Amazoniac Several people have shown me that paper when I asked for evidence that restriction of vitamin A improves psoriasis. I am sceptical. The authors note that most of the improvements and even complete clearing occured as early as 4/16 weeks after the start of the intervention. That's not nearly enough to significantly deplete retinol stores, especially on a diet that was low, but not insignificant in vitamin A, and it points to something more immediate.
Psoriasis is obviously not caused by excess vitamin A. People with psoriasis, in fact, tend to have lower levels of serum and hepatic retinol, and do not consume excess quantities of it. The underlying cause is found in other processes, and disturbances in the local retinol metabolites are an effect but not the cause of the problem. -
@Kvothe, a diet low in poisons leads to remission and returning with the normal diet results in relapse. Their supplementation without a change in diet does the same. Unless we assume that carotene metabolites are interfering with the action of poisonoic acids or it's disturbing the cell after being incorporated in fatty regions, we have to entertain the other options.
It wouldn't take a minimum of a month to notice the first positive effects from the exclusion of other irritants from the diet, but would match the decrease in circulating carotenes.