Studies showing cancer reversal / shrinking
-
@Mauritio said in Studies showing cancer reversal / shrinking:
I'm wondering where do heat shock proteins come into play here? They must be raised significantly...
I couldn't find peats newsletter on HSPs but here's the one on body temperature:
https://wiki.chadnet.org/body-temperature-inflammation-and-aging.pdfHere is a video that might be of interest.
#51: Heat Shock Proteins | Antibiotic Resistance | DHT Safety | Energy and Aging with Ray Peat, PhDIt has timestamps that do not automatically hotlink on this forum.
00:00 - Start
01:10 - Ray's new newsletter
05:05 - Le Chatelier's principle, Lamarckian fish, Barbara McClintock
09:18 - Gilbert Ling, ATP "the queen of cardinal adsorbents," phase transitions, coacervates, rigor mortis
13:51 - "The role of ATP is not limited to the contraction cycle. It dominates the physical state of muscle even in rest, keeping it soft and pliable... rigor mortis is but a lack of ATP..." Albert Szent-Györgyi
14:43 - Does the activation of the heat shock proteins (HSPs) precede cell division?
16:02 - Niacinamide and solubility, energy loss, DNA repair
19:09 - What about gelatin?
20:85 - Estrogen activates HSPs, redox balance, progesterone inhibits HSPs, water economy
23:15 - Should we activate the HSPs?
25:12 - Will the activation of the HSPs leave a scar?
27:06 - "Energy deprivation stabilizing proteins"
29:37 - Metallic taste in the mouth, lipid peroxidation
30:20 - "Estrogen, hyperventilation, lactate, etc., increase serotonin, and I think it’s serotonin that directly increases PTH, and then PTH increases NO." Ray Peat (2017)
33:30 - The living cell is more susceptible in the fatigued state
38:23 - HSP inhibitors: tetracycline, progesterone, methylene blue, etc.
38:58 - Is PTH a "newer" part of the system?
40:25 - Is RAAS more ancient than the HPA?
40:54 - Ray Peat's newsletter, Progest-E from Kenogen, Ray's history with progesterone
45:24 - Why can progesterone fill-in for the adrenals but pregnenolone cannot?
48:14 - Are pregnenolone and progesterone "true" hormones?
49:25 - If someone has a sensitive stomach -- how can they take progest-E?
50:14 - Ray's thoughts on using DHT and testosterone, gynecomastia, finasteride, governing principles of health
55:40 - Is DHT always "safer" than testosterone? Ray's thoughts on TRT
58:34 - What does Ray think of as a "max dose" of aspirin at one time?
01:00:04 - What happens to the agaratine in mushrooms? Does the mushroom water contain agaratine?
01:01:26 - How to distinguish between a fungal and bacterial infection?
01:07:40 - Does Ray prefer pure olive oil over coconut oil for the carrot salad and mushrooms? 1/2 a teaspoon provides a trace of PUFA
01:08:39 - Are fungal infections rarer than bacterial infections?
01:09:20 - H.pylori infection -- how to treat? Thoughts on dosing antibiotics
01:12:41 - The two-week time frame for antibiotic use scientific?
01:13:45 - Is antibiotic resistance important for the individual?
01:14:28 - Does antibiotic use cause a fungal overgrowth?
01:16:05 - Tetracyclines as antifungals? Inflammation predisposes to infection, feeling "uncomfortable" on minocycline
01:19:16 - Danny's experience on minocycline
01:21:46 - Question: why would a virus want to invade a cell?
01:29:28 - Viruses and weakened organisms
01:30:57 - Do viral pandemics exist?
01:36:02 - “...That is, if one pursues any ‘physical’ illness far enough and deep enough, one will find inevitably intrapsychic, intrapersonal, and social variables that are also involved as determinants.” Maslow (1993)
01:38:08 - What's the factor in the environment that's leading to frailty in young people?
01:40:42 - If a group has a problematic "death culture" holy book -- how can a functioning society be maintained?
01:44:54 - Could a holistic view of science be a foundation for a functional society?
01:45:51 - What is the long-term "artificial" struggle between humans?
01:47:10 - Does authoritarianism have anything to do with nature?
01:49:52 - Did the USA peak in the 1950s? The CIA's profound influence on culture
01:54:10 - Is technology a net-negative for sustaining a free culture?
01:55:25 - What about hierarchy in nature? Is it natural to rule over others?
01:57:52 - If an animal's needs were met, would they not express aggression? "Survival of the fittest," Pyotr Kropotkin
02:01:31 - What would be necessary factors to sustain cooperation among individuals?
02:02:44 - What is the most important news event that Ray is thinking about at the moment?
2:03:28 - The road to serfdom, dollar inflation, stock market manipulation
2:05:51 - Has anything become clearer about what will happen when a large portion of the US becomes jobless?
2:06:32 - Polarization in society (left vs. right, man vs. woman, etc.)
2:09:55 - What was the connection between Karl Marx and the Rothschilds?
2:12:07 - Was the 1917 soviet revolution controlled by Zionists? -
I foud Rays newsletter mentioning HSPs. It's called:
"Cumulative damage,
degeneration, & aging possibilities of reversal"Here's a few relevant quotes:
"...it occurred to me that it
would be good to consider what happens when the body temperature is increased by external heat, beyond the level at which the organism functions optimally. ""Partly, I’m thinking about the damage
that can be done by the increasing popularity of sauna treatments, and various kinds of “hyperthermic therapy for cancer,”"Independently, estrogen and nitric oxide are
known to promote fibrosis and cancer, and now the basic role of HSP in fibrosis (Bonniaud, et al.,2017) and cancer is being recognized, and the drug companies are creating a variety of HSP inhibitors."This quote I included because it's almost poetic and beautiful.
"...time is very relevant to the
organism—its present structure and properties reflect its previous states, and project its future tendencies and possibilities, its trajectory in life."Now this is the most relevant point, which the studies you posted corroborated so beautifully:
"At bedtime, a mild warm bath can compensate for low internal heat production, increasing the metabolic rate and helping to increase glycogen stores and increase progesterone level, making
deep restorative sleep possible. But if the bath is too warm or too prolonged, or if estrogen’s influence is too great, the increased metabolic rate can
Intensify the inefficient metabolism further depleting energy stores, and leading to higher stress hormones. Having extra carbohydrate before and during the warm bath improves its therapeutic function, and decreases the risk of heat shock." -
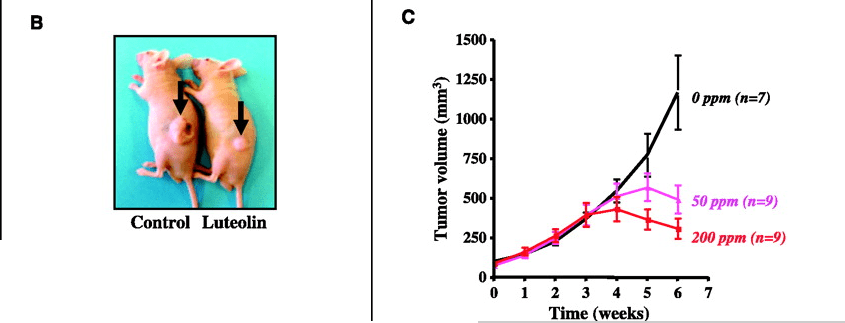
Very interesting human study on the effect of 60min. exercise (EX) vs. 60min hot bath at 40°C (PH).
Both were comparable in terms of elevating HSP70, but the elevation wasn't drastic and returned to baseline in about 2h.
The pro-inflammatory cytokine IL6 was elevated a lot more from exercise than the hot bath. So overall a hot bath seems to be safer than I thought and safer than exercise.
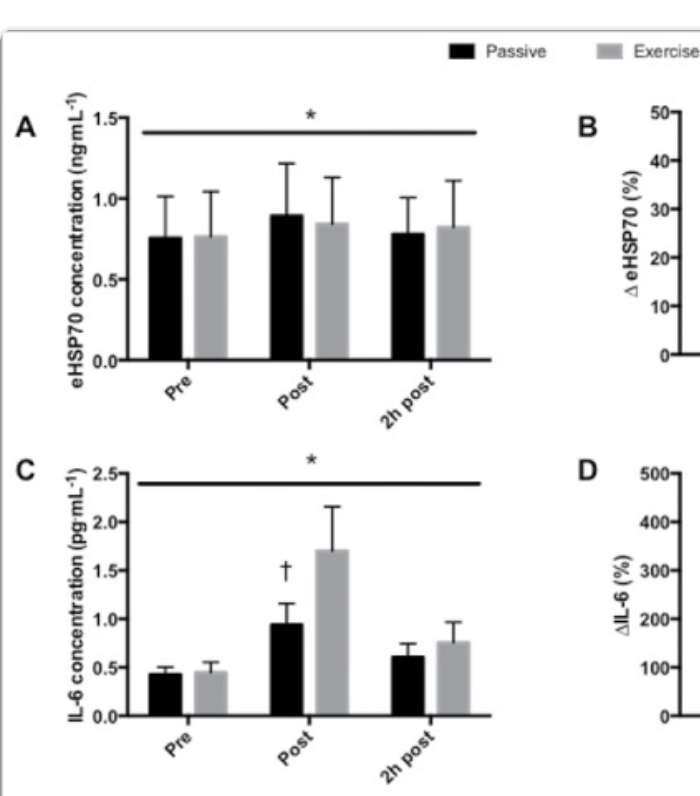
Interestingly just sitting in a hot bath for an hour increased their resting energy expenditure by 79%! That's what they found.
What makes the bath so good for tumors is the increase in temperature.
Both methods were comparable at raising core temperature.
But the bath was a lot better at increasing skin and muscle temperature compared to exericse!
https://pmc.ncbi.nlm.nih.gov/articles/PMC5605168/
@cs3000 @DavidPS -
 C cs3000 referenced this topic on
C cs3000 referenced this topic on
-
replied with more discussion on HSP at https://bioenergetic.forum/post/32387
-
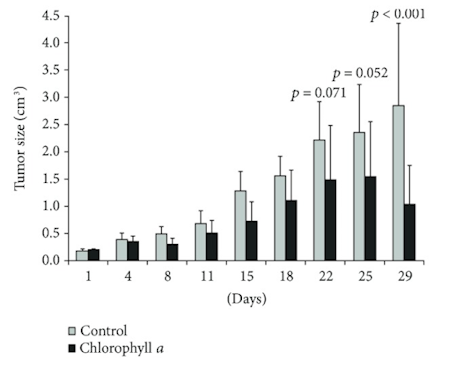
B-lapachone and breast cancer reversal when Nqo1 is expressed, (used 2 lines that dont have nqo1 then made them express nqo1, like a lot of cancers do maybe most)
Breakthrough dose was 70mg/kg every other day for just 5 uses (65mg/kg slowed a lot but didnt reverse interestingly). In one of the types (B) the cancer basically didnt even grow at all.
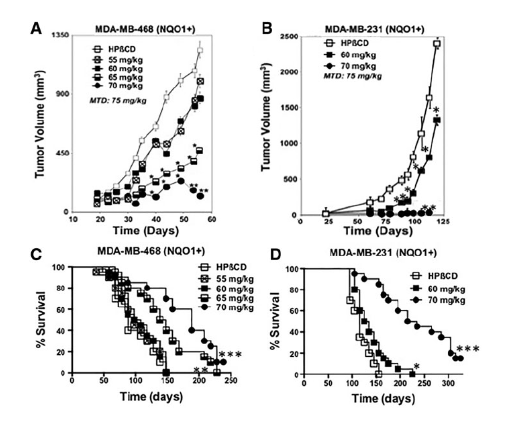
(would more treatments work for smaller doses?)
~(the effect relies on cells having NQO1 activity,
Cancer cells expressing >100 U of NQO1 enzyme activity are killed, while normal tissues that lack, or express low levels of, NQO1 are spared,
because high NQO1 metabolises the quionine into an unstable compound that causes a big surge in superoxide which generates h2o2 overload and kills the cell, shown at 4uM.
but the effect is somewhat selective on cancer cells vs healthy human cells which have less NQo1, at least up to 10 uM it doesnt kill at least some healthy cells measured. but does drastically inhibit proliferation of healthy cells >1uM.)in human breast cancer tissue microarrays,*60% (12/20) of breast cancer tissue samples showed strong NQO1 expression, while low to no significant expression wasnoted in adjacent normal breast tissue
NQO1 is a flavoprotein that is over-expressed approximately 5- to 200-fold compared with normal adjacent tissue in various solid tumors, including cancers of the pancreas, lung, prostate, and breast
~~But these are high and possibly toxic doses,
generally only 1mg/kg - 2.5mg/kg (~5mg-10mg human) are used for effects, maybe best at lower doses but regularly, combined with different things,~~considering the level of toxicity for NQO1 expressing tumors i'd wanna be extra sure there arent healthy tissues somewhere that express elevated amounts close to what cancers do , if using these high doses if theyre even reasonable to get ahold of, some healthy tissues express it to some extent eyes lungs etc https://doi.org/10.1016/S0891-5849(00)00310-5
~~here mice ate 70mg/kg in diet though and it showed beneficial effect on multiple measures in aging , and increased lifespan +17% in stress https://pmc.ncbi.nlm.nih.gov/articles/PMC3469505/#s3 but they didnt look at all tissues to see if theres damage,
I guess in food its less bioavailable mixing with other things so effectively a much lower dose (?)But here 80mg/kg orally just once showed signs of liver & kidney toxicity https://www.scielo.br/j/jbpml/a/6RX9dwWpVrnCVVFxp5gFjfr/?lang=en
The measured oral bioavailability of β-lapachone was 15.5%.
~~here 50mg/kg, injected i.p, but spaced out 1 day apart, for 10 treatments https://www.pnas.org/doi/10.1073/pnas.96.23.13369#sec-2 significantly lowered ovarian cancer and judging visually and by bodyweight didnt notice significant toxicity during this timeframe
**here ** 50mg/kg twice a day injected I.P increased mortality and was highly toxic https://www.tandfonline.com/doi/pdf/10.4161/cbt.4.1.1382 ,
Unlike the just 5 rounds dosing 1x every other day in the 1st studyβ-lapachone given for a dose of 50 mg/kg I.P. twice a day for two weeks was extremely toxic with nearly one-half of animals dying during the treatment.
{this might have been due to what they combined it with but maybe not}
Clearly complexation of β-lapachone with HPβ-CD increases the
bioavailability, efficacy, and toxicity of this active antipancreatic
cancer agent. Future studies to improve solubility with decreased
toxicity are warranted.and here 10mg/kg daily but injected into the blood for 1 - 2 weeks showed higher death rates https://www.scielo.br/j/bjmbr/a/pf9P7yD9qDP79yV5bDvPjqb/?lang=en
So the first study showed a survival increase doing just 5 treatments with a day apart. I guess you avoid lethal toxicity this way but idk how certain tissues would be affected , theres a tradeoff with that
I would only be happy using low dose for more treatments over time, if that had efficacy will see if i find anything
,
Lower dose 12.5mg or 25mg/kg subcutaneous daily https://www.nature.com/articles/s41598-017-02937-0#Sec2
slowed well but did not shrink alone
Lower doses orally, maybe ~5mg-10mg daily if not ~30mg human equiv, have a preventative effect on generating cancer. has a sedative effect https://www.sciencedirect.com/science/article/abs/pii/S0014299924001997
-
Human trial with methylglyoxal {aka pyruvaldehyde} (william Koch compound)
https://web.archive.org/web/20161017113947/http://www.cancer-therapy.org/CT/v4/B/HTML/17. Talukdar et al, 205-222.htmlLong term in a variety of cancers, ~80% of the people had remission or stability @dapose
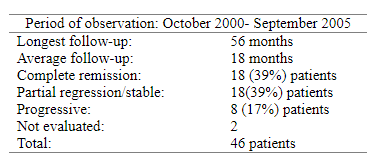
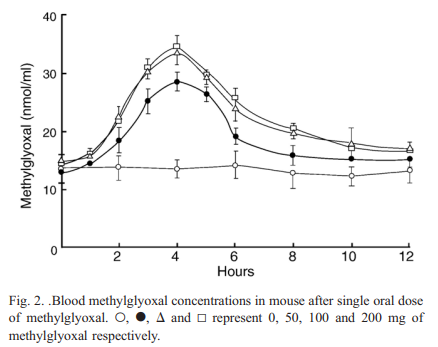
Its found in mankuna honey but the amounts they used here were high at ~500mg x4 a day (in water, just a little 60ml so dont tip pH too high?, with food) + vit c and some b vits, and over a long timeframe. seeing if i can find how long the effect should take. methylglyoxal levels go up with high blood glucose & finding glyoxalase 1 inhibitors to use should increase the effect for a lower dose needed https://www.cancertreatmentsresearch.com/methilglyoxal/ (nice writeup) looking up toxicity, apparently taking creatine can protect healthy cells so this has a selective effect
No significant toxicity (but can take creatine and vit C to enhance effect and protect healthy cells just in case there's toxicity on the heart without)
https://doi.org/10.1016/j.taap.2005.07.003Acute toxicity study was done with two species of animals, mouse and rat. The maximum dose of methylglyoxal for each mouse was for oral 2 g, for subcutaneous 1 g and for intravenous 0.3 g
All the animals except those used for biochemical studies (see below) were observed up to 90 days after completion of the treatment and were found to remain healthy. No toxic effect on physical condition and behavioral pattern such as hair texture, food intake etc. and death were observed. However, the subcutaneous injections appeared to be painful for both treated and control groups. {diluted in saline too} The pain appeared to persist for several minutes after injection.
In the animals, which received intravenous injections, swelling appeared in the tail and adjoining regions from 3rd week of the treatment. The swelling remained up to about 10 days from end of the treatment.
Treatment of methylglyoxal had no toxic effect on the
functions of liver, kidney and heart and hemopoietic organs
of the rats- As mentioned before, methylglyoxal had been found to possess strong antitumor activity. Szent-Gyorgyi and his associates and Apple and Greenberg long ago showed remarkable antiproliferative and curative effects of methylglyoxal towards cancer-bearing animals (Szent-Gyorgyi et al., 1967; Egyud and Szent-Gyorgyi, 1968; Apple and Greenberg, 1967).
- In in vivo and in vitro studies with animals and in vitro studies with a wide variety of human post-operative malignant tissue samples, we had observed that methylglyoxal acted specifically against malignant cells and ascorbic acid significantly augmented this anticancer effect of methylglyoxal (Ray et al., 1991, 1997a, 1997b; Biswas et al., 1997). Moreover, we had observed that creatine present in cardiac cells completely protected the animal from any possible deleterious effect of methylglyoxal treatment on cardiac mitochondria (Sinha Roy et al., 2003).
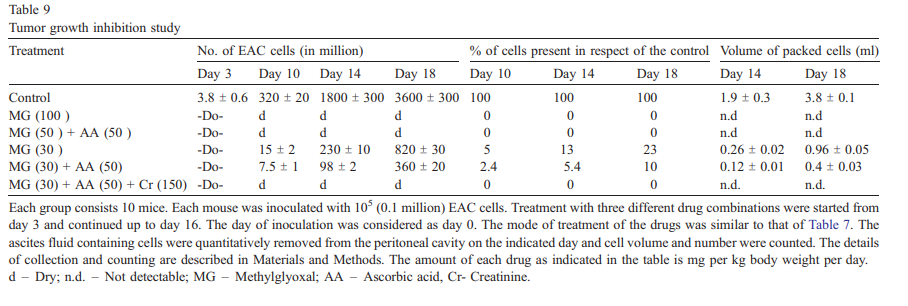
- So, we tested whether these compounds had any curative effect on mice inoculated with EAC cells. The results are presented in Table 7. It appears that at a particular dose the antiproliferative effect of methylglyoxal is augmented in presence of ascorbic acid and further improved when the mice were treated with methylglyoxal in combination with ascorbic acid and creatine. Nearly 80% of the animals treated with this combination were completely cured.
In mice 30mg/kg methylglyoxal slowed tumor development but 30mg/kg + 50mg/kg vit C + 150mg/kg creatine = 0 tumor development,
and regression into tumor free by day 10 but this was in tumors that just started growing
so gram amounts might not be needed if combined with creatine and vit C, was injected i.p so without food if thats tolerable, bumping up because of i.p ~300mg daily might be effective over time combined with 250mg vit C and 1gram creatine, split into 2 doses 6 days a week, maybe adding a couple more grams creatine would work better too
Creatine supplementation with methylglyoxal: a potent therapy for cancer in experimental models. Amino Acids, 48(8), 2003–2013. doi:10.1007/s00726-016-2224-1
20mg/kg but i.v + vit c + creatine (started on day 7,)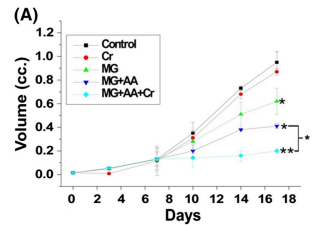
-
Very interesting . I guess the mechanism would be its oxidizing effects?
Ray talked about it a few times in his newsletter and it didn't sound positive.
Also methylglyoxal is a naturally occuring of glycolysis (not oxidative phosphorylation) so it should be higher in unhealthy people . Plus it can be converted into lactate, which is the body's way of detoxing it.When you read studies on it, it doesn't sound encouraging, it's seen as cause of diabetes and other illnesses.
Shouldn't it be very good for diabetes if it's so pro-metabolic ? Maybe it rises as a defense mechanism ."...MGO is linked to the development of diabetes, vascular complications of diabetes, and other age-related diseases."
https://pubmed.ncbi.nlm.nih.gov/31539311/Methylglyoxal is a major cell-permeant precursor of advanced glycation end-products (AGEs), which are associated with several pathologies including diabetes, aging and neurodegenerative diseases.
https://pubmed.ncbi.nlm.nih.gov/25709564Then there's this quote by Peat.
https://raypeatexplained.com/ray-peat-on-oxidation/#152124319605143112494046561751189594877And this study showing dietary intake being associated with less low grade Inflammation.
https://pubmed.ncbi.nlm.nih.gov/36055771/ -
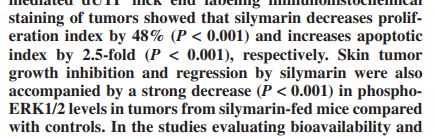
@Mauritio its an aldehyde so doesnt sound like a healthy compound / pro metabolic outside of specific use nah (probably best not to take generally outside of cancer) so its one of those things that has an outweighing effect on cancer cells, the anti-cancer dose didnt show toxicity though so i guess healthy cells can deal with that amount well enough but probably some extra burden
apparently low amounts can stimulate cancer growth but higher amounts triggers the apoptosis process (thats normally lacking because of damage making it inefficient, and pH change, needs to be more acidic inside the tissue for apoptosis to happen optimally, cancers are acidic nearby but higher end pH inside - maybe methylglyoxal accumulation makes the tumor more acidic?)
Also it has two carbonyl groups , koch and reinstorff back in the day thought these can be used to take out things with strong bonds that are sticking around blocking mitochondria respiration and enable healthy processes again. maybe @dapose has more to to say on that
Following Glo1 inhibition, cancer cells switch from glycolysis to tricarboxylic acid (TCA) cycle to avoid apoptosis induced by MGO accumulation.
for some reason cancer cells are more sensitive to MGO overload than normal ones even though they have higher glutathione (which sounds to me like the effect is less about damage and more about re-enabling apoptosis unless for some reason they accumulate extreme amounts) https://www.science.org/doi/10.1126/science.160.3832.1140.a
-
@cs3000 ok thanks.
-
I feel like oleocanthal and oleurupin deserve more attention.
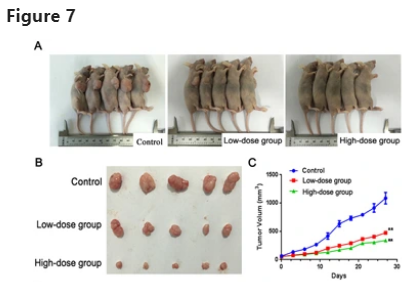
Check this out. 97% reduction in cancer growth in-vivo!
Mostly by inhibiting estrogen.
But it's also been shown to be effective in other cancers.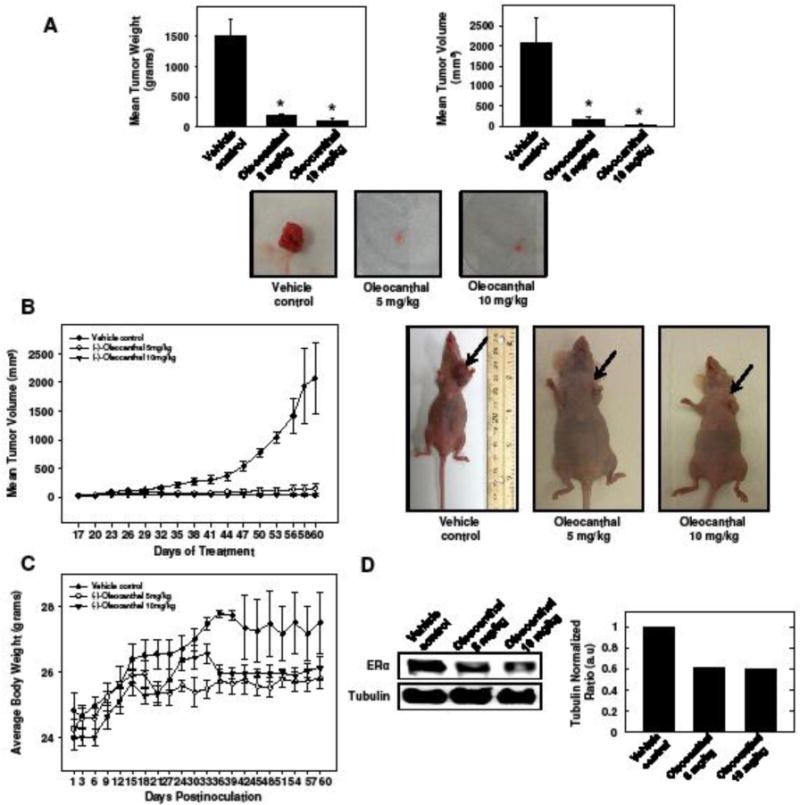
"Treatment with 5 mg/kg or 10 mg/kg (−)-oleocanthal resulted in 97% inhibition of tumor growth in orthotopic athymic mice bearing BT-474 tumor xenografts compared to vehicle-treated animals. (−)-Oleocanthal treatment reduced total levels of estrogen receptors in BT-474 cells both in vitro and in vivo. "
"Anticancer activity of (−)-oleocanthal has been demonstrated in different tumor types including breast carcinoma, prostate carcinoma, hepatocellular carcinoma, colon cancer, melanoma, and multiple myeloma (Akl et al., 2014; Elnagar et al., 2011; Fini et al., 2008; Fogli et al., 2016; Pei et al., 2016; Scotece et al., 2013)"
-
farcarinol (from carrots and related plants like ginseng) and related compounds for colon cancer
also knows as panaxynol or carotatoxin
interestingly-- the nrf2 stimulating activity is apparently higher in relevant dietary doses from carrots than it is from cruciferous vegetable. another contradiction in the peater world
-
-
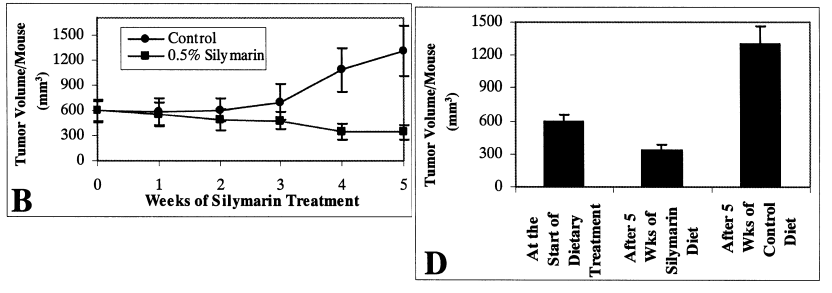
1 haidut posted before:
BRAF + MEK inhibition therapy {inhibiting MAPK through selective paths} + the doxycylcine antiobiotic = regression in a person who had metastasised melanoma into liver & bile duct
https://pmc.ncbi.nlm.nih.gov/articles/PMC4699264/
https://rupress.org/jem/article/218/9/e20210571/212494/Activation-of-the-integrated-stress-responsealone didnt do much , but helped delay the eventual resistance seen in the yellow line
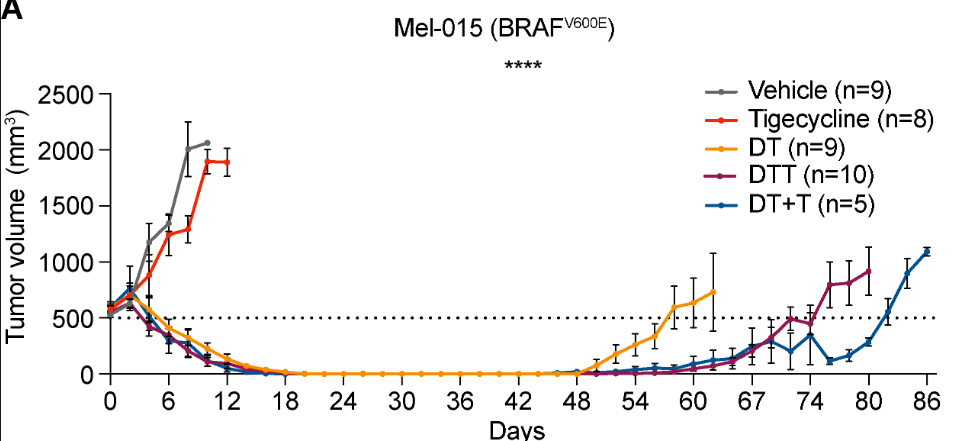
In the person it gave full remission as doxycycline + the mapk inhibitors
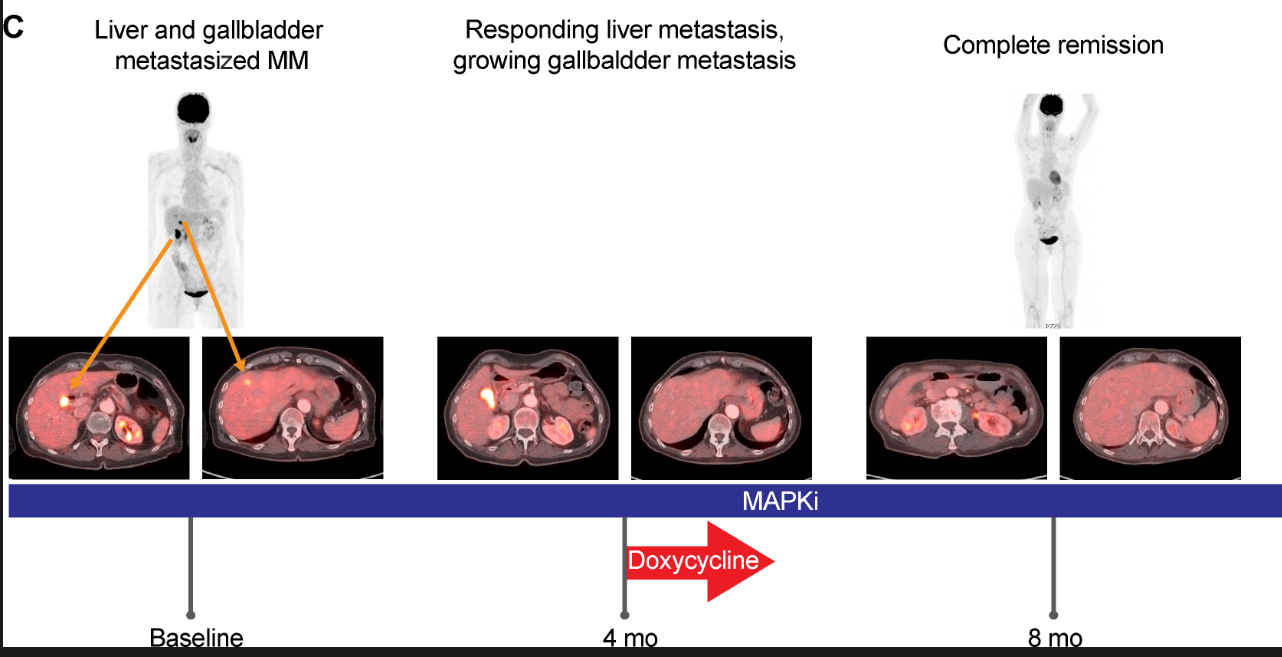
To assess the relevance of our in vitro and preclinical findings, we followed the clinical course of one 73-yr-old female patient at our clinic. The patient was diagnosed with stage III melanoma in 2011 and with a relapse of her disease in 2016 after an episode of jaundice, which was related to a tumor mass in her gallbladder and bile duct.
the presence of brown pigment associated with these cells was highly suggestive for a melanoma metastasis.
Subsequently BRAF-MEK inhibitor therapy was initiated. Response assessment after four cycles showed that while the liver metastasis had responded to the treatment, the gallbladder did not.
Due to a skin infection (an acne-like rash) the patient received doxycycline during her fifth BRAF-MEK inhibitor cycle for a total of 12 d.
Strikingly, the gallbladder metastasis started to regress after six cycles, as measured by CT scan, and the PET-CT scan after eight cycles showed a complete response. The patient was under BRAF-MEK inhibitor therapy and had a persistent response for >36 mo (Fig. 6 C). This particular case study highlights the potential clinical benefit of using tetracyclines to sensitize intrinsically resistant lesions to MAPK inhibitors.*Lipoic acid is a mapk inhibitor, and showed decent effects slowing tumors alone i posted in the first post.
https://onlinelibrary.wiley.com/doi/10.1155/2022/1894379ALA inhibited a variety of mitogen-activated protein kinase (MAPK) signaling pathways in the epithelial cells
So i wonder if a combo of lipoic acid + doxycycline could be good for giving regression of melanoma / metastasised melanoma to other areas
50 - 150uM is too high to hit in vivo probably, its like 20ug/ml blood i think
so maybe for topical applied to melanoma as the combo. lipoic acid can penetrate if absorbs in right thing, propylene glycol or heated mct oil. not sure about doxycycline . But short half life on lipoic so would have to get a lot in
https://pmc.ncbi.nlm.nih.gov/articles/PMC3648887/ here they got 14ug/cm2 to pass through normal skin
but melanoma = melanocytes so i guess easier to penetrate as doesnt have the outer SC layer?
maybe theres something else for systemic use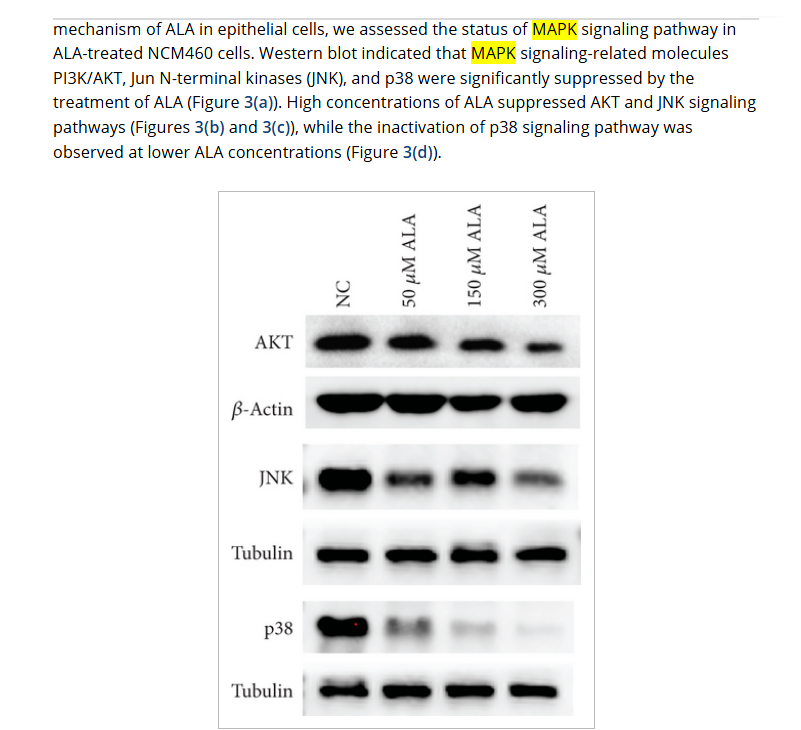
extra: (not showing remission but metastasis effect)
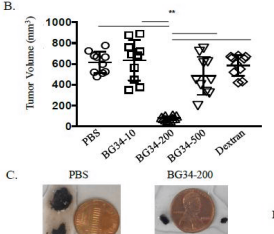
B-Glucan (particulate) melanoma matastasis prevention
https://www.researchgate.net/publication/327193765_Beta-glucan-induced_inflammatory_monocytes_mediate_antitumor_efficacy_in_the_murine_lung
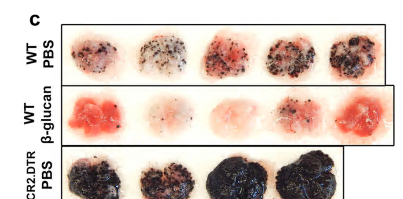
oat b-gluten best effect at 200kda size
https://www.researchgate.net/publication/320392541_Systemic_Administration_of_bglucan_of_200_kDa_Modulates_Melanoma_Microenvironment_and_Suppresses_Metastatic_Cancer
turkey tail glucan is 100kda https://pmc.ncbi.nlm.nih.gov/articles/PMC10000499/
Feeding inhibition effect (but is anti androgen)
https://pubmed.ncbi.nlm.nih.gov/26408688/ -
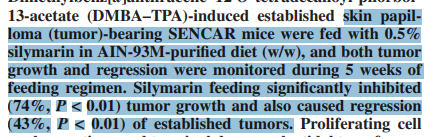
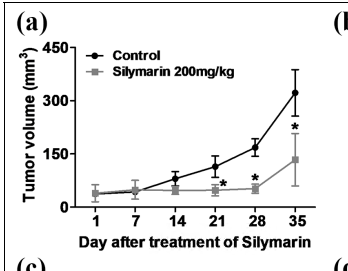
Another showing regression of existing tumors
human squamous cell carcinomaFeeding high amounts of silymarin
(note silymarin / milk thistle inhibits thyroid hormone transport, not suitable for general use)Shrank the pre existing tumors
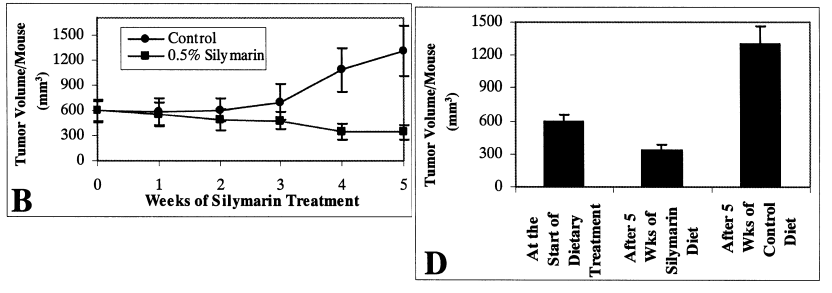
doi.org/10.1093/carcin/23.3.499
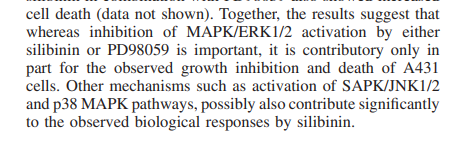
melanoma, 500mg/kg ~ 3g human only using 1 dose every 2weeks slowed
but didnt regress (maybe lower dose more often could have too)
10.1002/mc.22208
200mg/kg 5days a week for 5 weeks , didnt show kidney or liver toxicity 10.1177/1010428318776170
stalled growth in an oral tumor until the end, but didnt get to regression
Can penetrate skin in Propylene glycol and stays in skin cells for long while https://www.sciencedirect.com/science/article/abs/pii/S0378517322009863
glycerol / glycerine increases growth of some tumors so probably not appopriate as to use for entry
https://pmc.ncbi.nlm.nih.gov/articles/PMC8908677/Propylene glycol is different. maybe some connection but is used as penetration enhancer in anti tumor studies with effect still so
https://pubmed.ncbi.nlm.nih.gov/23186833/Mct oil might be good if it dissolves well, warmed in a saucepan
-
@cs3000
450mg daily created regression in this persons liver tumor, to half its size. but the effects stalled and it re-grew after around a year
https://pmc.ncbi.nlm.nih.gov/articles/PMC2769275/Ultrasonography in our outpatient department revealed a large tumour with central necrosis, measuring about 11 cm in diameter,
CT scan of the liver was performed again and revealed HCC regression, with tumour size reduced to about 4.6 cm in diameter, and portal vein thrombosis (Figure 3).
Silymarin 450 mg daily was the only regularly prescribed medicine during HCC reduction.
The tumour size did not contract persistently as shown by abdominal echo. CT scan of the liver was performed prior to the surgery, revealing an HCC size similar to the previous readings and portal vein thrombosis.@cs3000 said in Studies showing cancer reversal / shrinking:
Another showing regression of existing tumors
human squamous cell carcinoma
Feeding high amounts of silymarin
( note silymarin / milk thistle inhibits thyroid hormone transport, not suitable for general use)
Shrank the pre existing tumors
-
Natural compound Physachenolide C (but not commercially available yet) gave complete remission in melanoma. in 1/3 of the mice it stayed regressed. (in the other 2/3, maybe doxycycline could have brought back the effect)
its a highly potent BET inhibitorhttps://pmc.ncbi.nlm.nih.gov/articles/PMC8571524/#sec0011
enhanced immunotherapy for regression (enhance with b-glucan?)
https://pmc.ncbi.nlm.nih.gov/articles/PMC8802328/#S19 -
interesting find - if u target a main 2% subset of melanoma cells the tumor goes in most cases without destroying the other part. if some are left theres potential for the regression to return
(does doxycyline help these ones get destroyed when combined with inhibitors?)https://www.pnas.org/doi/10.1073/pnas.1009069108
we revealed that established tumor lesions can be efficiently eradicated by targeted elimination of the less than 2% subset of melanoma cells with the CD20+ high molecular weight melanoma-associated antigen (HMW-MAA)+ phenotype without targeting the tumor cell mass, whereas targeted elimination of any minor subset is less effective.
These data provide a strategy for improving the biological therapy of melanomas and, moreover, for redesigning current drug development paradigms used in the treatment of cancer.HMW-MAA+ cells gave rise to melanomas upon transplantation, whereas sorted HMW-MAA− cells from the same melanoma did not.
indicating that these cells exhibit melanoma-initiating capacities.
T cells with redirected specificity for CD20 eradicated established melanoma lesions in four out of five melanoma biopsies, although the targeted cells represented less than 2% of melanoma cells.
It is noteworthy that transplanted tumors of patient 5, in which no CD20+ melanoma cells were detected, could not be eradicated by a CD20-redirected T-cell attack.Where tumors were eradicated, no tumor relapse occurred during the observation period of >36 wk.
Because no tumor relapse was observed in any case during the >36 wk observation period, such melanoma eradication is obviously long lasting
We conclude that CD20 is not functionally crucial but marks a specific cell population. The unexpected observation, however, is that targeting the minor CD20+ melanoma cell population is as effective as targeting the majority of tumor cells. A caveat for a broad therapeutic application is that obviously some melanomas, in our cohort one out of five patients, do not harbor CD20+ melanoma cellsThe observation that the specific elimination of a minor subset of tumor cells results in eradication of established melanoma lesions is crucial for the understanding of the biology of melanoma. Continuous melanoma growth obviously requires the presence of a minor population of cells, which displays the CD20+ HMW-MAA+ phenotype;Elimination of these cells is obviously required to eradicate the melanoma irrespective of the bulk of tumor cells
-
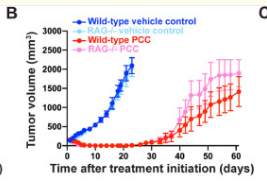
@cs3000 WIlliam Koch the chemistry of natural immunity, cases at the bottom pages showing amazing recoveries
@cs3000 said in Studies showing cancer reversal / shrinking:
Human trial with methylglyoxal {aka pyruvaldehyde} (william Koch compound)
https://web.archive.org/web/20161017113947/http://www.cancer-therapy.org/CT/v4/B/HTML/17. Talukdar et al, 205-222.htmlLong term in a variety of cancers, ~80% of the people had remission or stability
, -
@cs3000 Nice, was that just methylglyoxal. Or also 6 months of vegan , low protein diet ?
-
@Mauritio all of it combined probably with methylgloxal being the main effect, maybe the low protein helps improve response rate,
In the modern trial ~40% of the people got complete remission of their tumors taken orally daily, without dietary changes mentioned just added vitamin C. Koch injected it just 1 time into muscle, then waited a couple weeks and repeated that twice more if needed
they tested some other stuff with efficacy on animals (human study mentioned low toxicity for the methylgloxal tho when done in vivo and as just methylglyoxal form)
other ones , they're "unsaturated diketones" or things that form them as "peroxides of substances that liberate free carboyl groups to form the unsatured diketone"
"Unsaturated diketones are organic compounds containing two ketone (carbonyl, C=O) functional groups and one or more double or triple bonds within their molecular structure. These unsaturated bonds make the molecule chemically reactive and allow for unique properties."
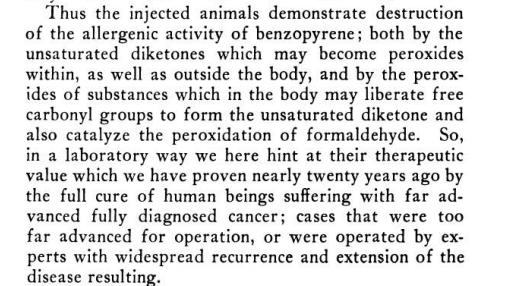
Something interesting, some of those substances create carbon dioxide when they degrade. or relates in some way
Quinones are unsaturated diketones
part of curcumin molecule is an unsaturated β-diketone https://casereports.bmj.com/content/2017/bcr-2016-218148 but generally they havent shown remission like the methylgloxal
some ketones like acetylacetone