Conditional problems with vitamin A: a place for sane discussions
-
Co-adjuvant effects of retinoic acid and IL-15 induce inflammatory immunity to dietary antigens
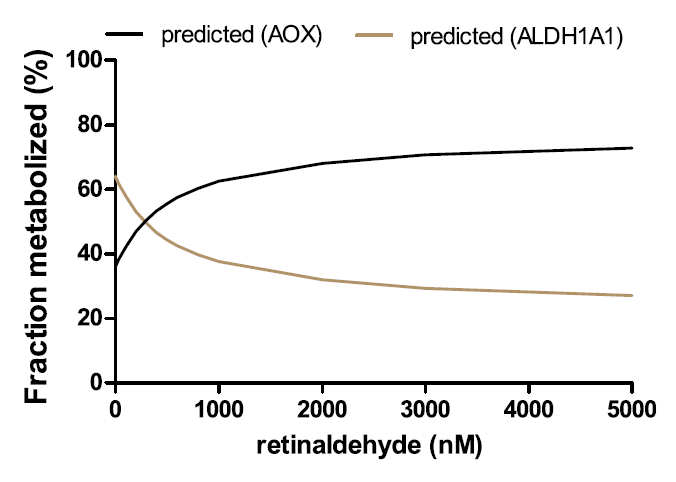
"Here we find in mice that in conjunction with IL-15, a cytokine greatly upregulated in the gut of coeliac disease patients[3,7], poisonoic acid rapidly activates dendritic cells to induce JNK (also known as MAPK8) phosphorylation and release the proinflammatory cytokines IL-12p70 and IL-23."
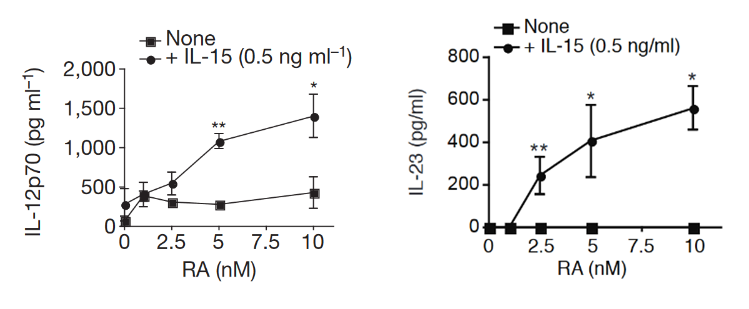
"Our study reveals that in the presence of IL-15, RA has unforeseen co-adjuvant properties that induce TH1 immunity to fed antigens (
Fig. 4f). It indicates further that under infectious conditions associated with induction of IL-15 and IL-6 in the intestinal mucosa, RA will also promote TH17 immunity. These observations caution against the use of poison A and RA for the treatment of autoimmunity and inflammatory intestinal disorders associated with high levels of IL-15. Indeed, a causal relationship between retinoids used for the treatment of acne and inflammatory bowel disease has been implicated in a subset of patients[25].""More generally, our study supports the concept that there are no ‘unconditional’ suppressive factors, and that integration of tissue and exogenous signals determine the class of the immune response, which ultimately needs to be tailored to the tissue and the antigen. In line with the idea that the same proinflammatory factors trigger different immunological outcomes depending on the tissue in which they are induced, we found that the ability of IL-12 to inhibit Treg-cell induction was blocked by butyrate, a metabolite produced by commensal bacteria present in the colon but not in the small bowel (data not shown)."
"Our observations may also explain why oral tolerance is disrupted in patients with inflammatory bowel disease[28] who also have dysregulated IL-15 expression in the gut[29]. Lastly, our results indicate that inhibiting IL-15 signalling may constitute a therapeutic intervention to restore mucosal tolerance to luminal antigens."
Insights into the Pathogenesis and Treatment of Psoriasis
"[..]dendritic cells and effector T-cells are important in the development of the psoriastic lesion, and cytokines produced by these cells stimulate keratinocytes to proliferate and increase the migration of inflammatory cells into the skin, promoting epidermal hyperplasia and inflammation (Monteleone, G. et al., 2011)."
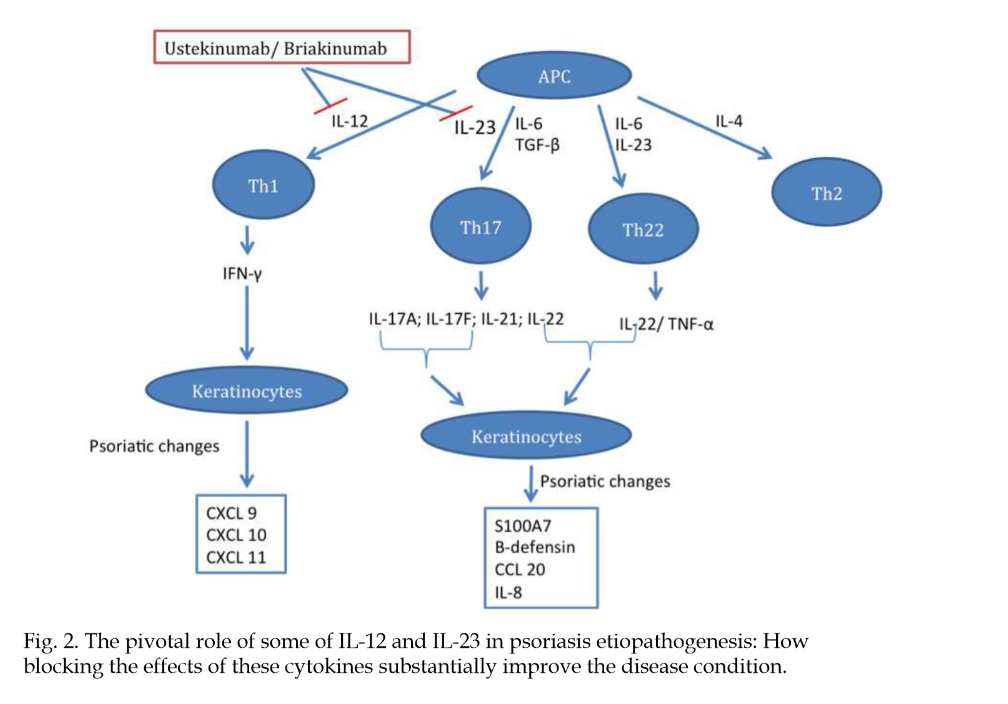
"An increase in efficacy and reduction of adverse events are the main drivers for new therapies. Infections, one type of adverse event, usually increase in patients receiving anti-cytokine therapy (Dinarello, 2003)."
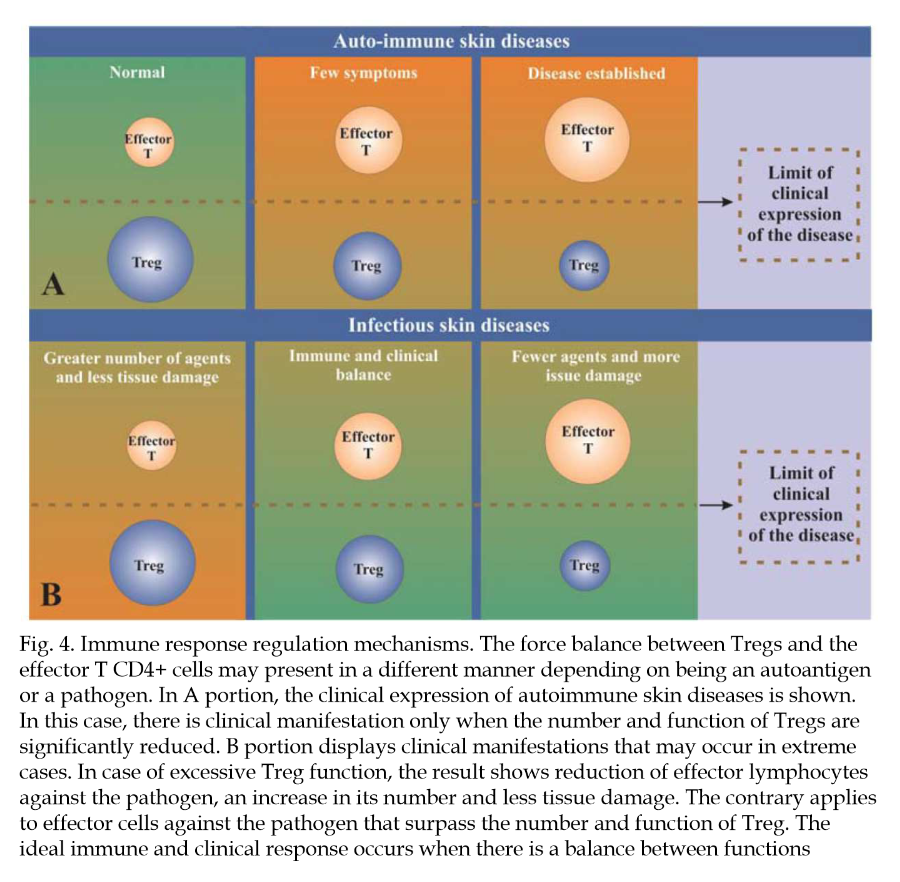
"Some inflammatory agents, whether physical, chemical, or infectious, induce an intense immune response. This immune response against them frequently results in tissue damage that could be more intense if it were not for the interference of regulatory mechanisms (Belkaid et al., 2006). As has already been specified, Treg cells help limit the damage caused by a vigorous immune response."
"Similarly, excessive activity of Treg cells may limit the magnitude of the immune response, which may result in failure to control an infection. On the other hand, the absence of the T regulator may result in intense inflammation and autoimmune dermatitis. Tissue damage may also result from the development of effector cells against their own auto-antigens (Figure 4)."
"An improved understanding of the role of T regulators in psoriasis may lead to the identification of new targets for treatment. More specifically, the goal is to manipulate natural regulator cells or those induced by means of an increase or decrease of their function, depending on the circumstances."
Immunopathogenesis of inflammatory bowel disease
"Altered gut permeability may lead to increased bacteria adherence and inappropriate exposure of the mucosal immune system to bacterial products causing inflammation."
"Negative regulation of the host innate immune responses to the indigenous microflora maintains gut homeostasis. Key players in the negative mucosal regulation include interleukin-10 (IL-10) and IL-2, as evidenced by mice with deficiencies in these factors develop spontaneous intestinal inflammation, but are protected from intestinal disease when raised in germ-free environments[77–>79]. This indicates that at steady state, pathologic consequences of immune activation by commensal microflora are constitutively inhibited by IL-10 and -2 dependent mechanisms."
"A subset of T cells producing IL-6 and IL-17, now known as Th17 cells, has emerged as an important mediator of the T-cell response in gut inflammation (Figure 4)."
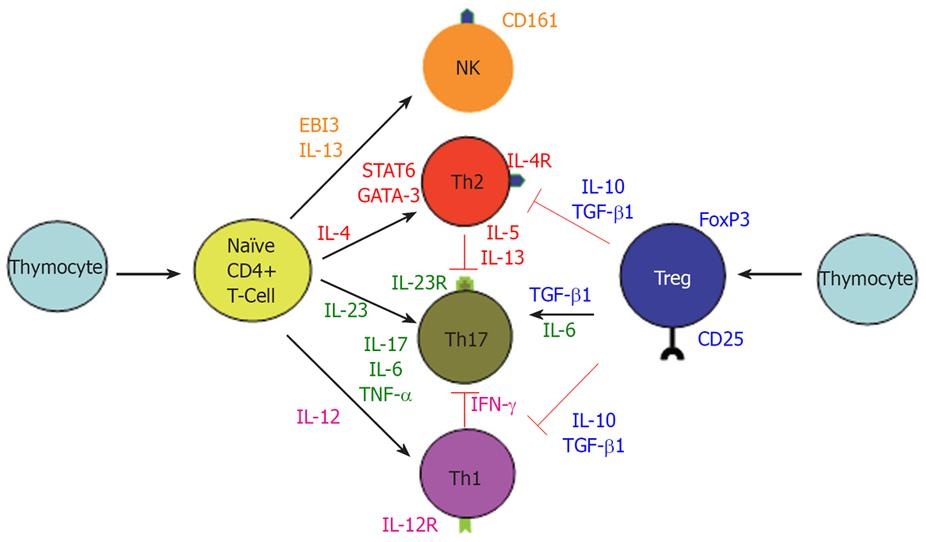
"The above findings do not exclude the role of exaggerated Th1 response in CD since IL-12/IFN-γ and IL-23/IL-17 may be parallel pathways involved in inflammatory response. Interestingly, IL-12/IFN-γ and IL-23/IL17 pathways are mutually exclusive, since IFN-γ suppress IL-17 and vice versa (Figure 4)[104]. It is of pathogenic importance to consider all of the major immune pathways that are responsible for the development of CD. For example, therapeutic targeting of only the newly discovered IL-23/IL-17 immune axis may actually exacerbate CD by accelerating the IL-2/IFN-γ Th1 pathway."
-
@Amazoniac
I hope others will contribute to this thread re absorption and clearance rates as well as mechanisms by which vit A may be poisonous/problematic. Are you personally limiting vit A intake at this time?I’m not (yet). Given what’s going on at RPF, I have, if anything upped eggs/milk/pumpkin/etc in my diet over the last few months to celebrate high-metabolic-rate good health, Ray Peat style, as quiet dissent. Like Amazoniac, I think it’s good for us to remain open to new information as it arises, however, about any potential problems associated with excessive vit A intake.
Might I get your advice based on my brief personal history, which was unusually high-dose vit A for several reasons? Growing up in the 1970s, my mom became a health-food nut and both mom and dad took – and gave me as a child – a large volume of vitamin supplements. From the age of 3 onwards (maybe through puberty), I was encouraged to take a daily beta-carotene supplement. We drank lots of carrot juice. The soles of my feet had an orange tint, which my doc may have even commented on once. We kept up this extraordinarily high diet + supplement regimen until I was a teenager. I took a round or two of Accutane for acne as a 17 year old. Under lots of other stressors and chronic sleep deprivation, I was diagnosed as a type-1 diabetic at age 20, which ran in my half-Norwegian family. I would be a likely candidate to have had – and very likely still have – excessive vit A stored in liver, adipose and elsewhere. Do you think I should try the low vit-A diet? (I can’t believe I’m actually writing those words…!!!...rest assured, only as a speculative hypothesis and not a likely action plan.)
-
@T-3
Adding: I never had (and don't think I have at present) any vit A toxicity symptoms. The callouses on my feet and palms are probably a bit more "orange tinted" than most people's and my complexion is noticeably darker than either of my parents, but I also get a lot of healthy sun exposure. My default is skepticism toward the hypothesis that I suffer from vit A toxicity. Eating high-vit-A foods makes me feel good and I don't think I have any problems associated with those foods. Thus, I'd say that worrying about vit A intake would be creating a pseudo diet problem where none in fact exists. But I gather that Amazoniac has made this thread because he has some concerns about vit A in his own diet, or is that wrong? -
https://www.bioenergetic.life/clips/8442a?t=813&c=17
"So a lot of these oils that are purported to be good for our health are actually quite thyroid toxic and long-term use could lead to conditions that are common in low thyroid and is as detrimental as cancer. Yeah. And there's one which isn't really a fatty acid, but it's a highly unsaturated molecule, carotene, which is the precursor to vitamin A. It not only blocks the cellular sites that use vitamin A, but as a polyunsaturated molecule, it also blocks the thyroid function every place that the vegetable oils do."
-
@DavidPS Thanks for posting this quote from Ray. Apropos! DavidPS, are you limiting eggs, oranges, persimmons, pumpkin, sweet potato and the like?
Is the retinol in milk different from the beta carotene in orange colored foods?
I think I'm asking embarrassingly basic questions here. And I worry my advice request may inadvertently be derailing what Amazoniac wanted this thread to be about. I just wanted to get expert advice re practical take-aways from those of you thinking carefully about the evidence base from published studies regarding risks of excessive retinol and/or beta-carotene-containing foods. Has what you've learned about vit-A risk changed the way you eat?
-
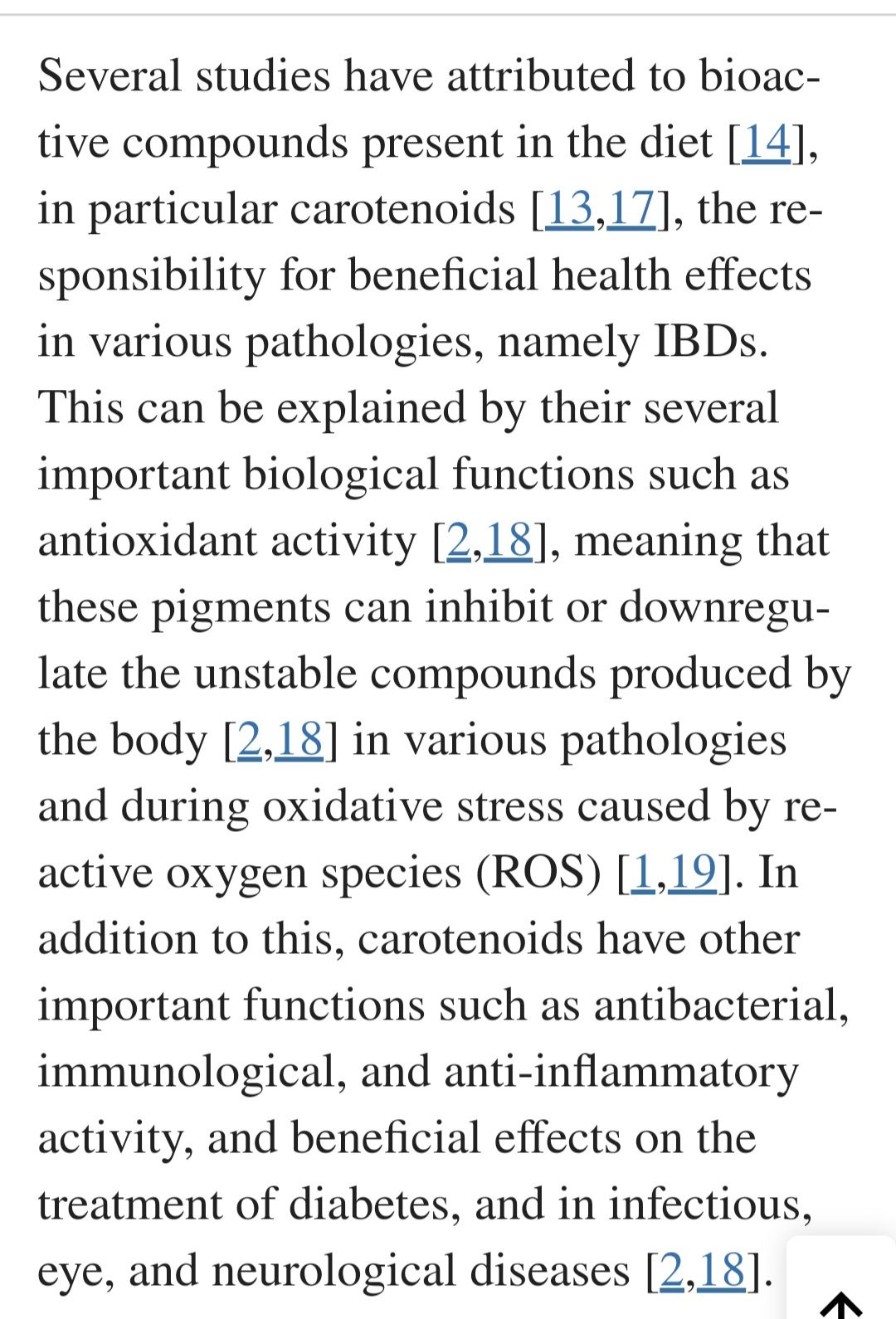
Most here are familiar with RP's discovery that a daily carrot salad made him feel better. Some think it was because of the "colon sweeping" effect, but if that were the case, wouldn't charcoal have the same effect? Could it be because Beta carotene is an effective modulator of the gut biome?
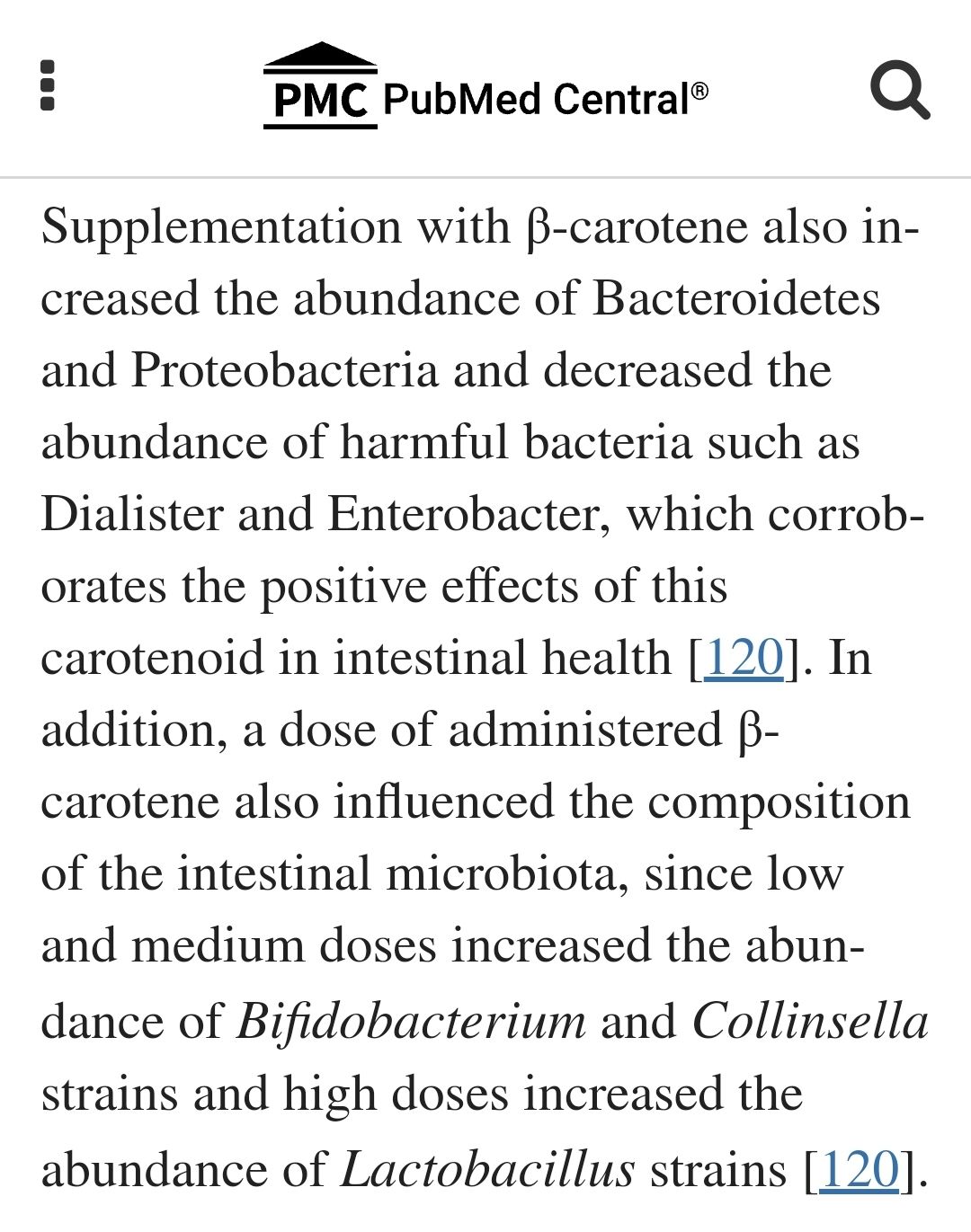
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10220829/
-
@S-Holmes
-
@T-3 - Thanks for your kind words. I am trying to make sense of it all. Danny Roddy helped me understand that vitamin A is essential (that why it is a vitamin) and has a recent video (3 minutes) that discusses its role making hormones in the body.
In addition, Dr Peat wrote in his article, BSE - mad cow - scrapie, etc.: Stimulated amyloid degeneration and the toxic fats:
"The amyloidoses affect different tissues in different ways, but when they occur in the brain, they produce progressive loss of function, with the type of protein forming the fibrils determining the nature of the functional loss. The protein which carries thyroid hormone and vitamin A, transthyretin, can produce nerve and brain amyloid disease, but it can also protect against other amyloid brain diseases; in Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, and the “prion diseases” (scrapie, kuru, CJD, BSE, etc.) amyloid particles are formed by different proteins. The transthyretin protein which is binding small molecules resists condensation into the amyloid fibrils, but without its normal vitamin A and thyroid hormone, it can create toxic fibrils. (Raghu, et al., 2002.)"
I found that passage to be scary. One does not want to go too low in vitamin A. I get mine from real foods and I do not limit my consumption based on vitamin A. I do not use vitamin A supplements and topical A may be counterproductive.
Enhancement of chemical carcinogenesis in the hamster cheek pouch by prior topical application of vitamin A palmitate -
@S-Holmes said in Conditional problems with vitamin A: a place for sane discussions:
Most here are familiar with RP's discovery that a daily carrot salad made him feel better. Some think it was because of the "colon sweeping" effect, but if that were the case, wouldn't charcoal have the same effect? Could it be because Beta carotene is an effective modulator of the gut biome?
I can share, anecdotally, that carrot salad always helps me, charcoal does not, with regard to transit time and moving the train down the tracks. I believe the carrot salad's effectiveness is due to the mere mechanics of the fibrous carrot moving through your system. At least that is how it feels to me.
-
@T-3 said in Conditional problems with vitamin A: a place for sane discussions:
@Amazoniac
I hope others will contribute to this thread re absorption and clearance rates as well as mechanisms by which vit A may be poisonous/problematic. Are you personally limiting vit A intake at this time?I’m not (yet). Given what’s going on at RPF, I have, if anything upped eggs/milk/pumpkin/etc in my diet over the last few months to celebrate high-metabolic-rate good health, Ray Peat style, as quiet dissent. Like Amazoniac, I think it’s good for us to remain open to new information as it arises, however, about any potential problems associated with excessive vit A intake.
Might I get your advice based on my brief personal history, which was unusually high-dose vit A for several reasons? Growing up in the 1970s, my mom became a health-food nut and both mom and dad took – and gave me as a child – a large volume of vitamin supplements. From the age of 3 onwards (maybe through puberty), I was encouraged to take a daily beta-carotene supplement. We drank lots of carrot juice. The soles of my feet had an orange tint, which my doc may have even commented on once. We kept up this extraordinarily high diet + supplement regimen until I was a teenager. I took a round or two of Accutane for acne as a 17 year old. Under lots of other stressors and chronic sleep deprivation, I was diagnosed as a type-1 diabetic at age 20, which ran in my half-Norwegian family. I would be a likely candidate to have had – and very likely still have – excessive vit A stored in liver, adipose and elsewhere. Do you think I should try the low vit-A diet? (I can’t believe I’m actually writing those words…!!!...rest assured, only as a speculative hypothesis and not a likely action plan.)
@T-3 said in Conditional problems with vitamin A: a place for sane discussions:
@T-3
Adding: I never had (and don't think I have at present) any vit A toxicity symptoms. The callouses on my feet and palms are probably a bit more "orange tinted" than most people's and my complexion is noticeably darker than either of my parents, but I also get a lot of healthy sun exposure. My default is skepticism toward the hypothesis that I suffer from vit A toxicity. Eating high-vit-A foods makes me feel good and I don't think I have any problems associated with those foods. Thus, I'd say that worrying about vit A intake would be creating a pseudo diet problem where none in fact exists. But I gather that Amazoniac has made this thread because he has some concerns about vit A in his own diet, or is that wrong?The terms 'macabrotenoids' and 'poisonoids' are for fun. It used to be clear early on, but the poison A crowd took the confusion to proportions that may create doubt for some people on whether these are humorous or not.
You can find a report (on the main poison A thread of the Garrey Smeat Forum) from researchers who found that people with diabetes and hypothyroidism were groups that had unusually elevated stores of poisonol. What increases the metabolic rate tends to also increase the internal consumption of poison A, and reserves can be normalized this way rather than through restriction.
I think that the community has to separate excess poison A stores from its toxicity. Lumping them invariably together contributes to the pro-poison A and
anti-poison Apro-life camps going on futile debates.The person doesn't have to be overloaded with poison A in the body to experience toxicity problems, these can happen at low intakes when the metabolism of a substance is deranged or if its addition influences pathways that are maladjusted (⇈).
And we don't know when it's really a maladjustement, making avoidance risky. The elevation of poisonoids may be containing an infection or inhibiting cancer. If the immune system is suppressed, it can represent easing on a battle, forcing the body to find ways to internalize the problem and minimize the associated cost.
One of the sources of poison in the gut is what recirculates through bile, that may contribute to local problems as dietary poisons do, but what's framed as 'detoxification events' can be the body transitioning from aggressive mode to tolerance. Something of this nature would align with people suddenly being able to not overreact to foods that used to cause trouble.
In the previous post, the authors pointed out that inhibition of specific inflammatory proteins carries risks (despite improvements). I suppose that it's riskier to try to inhibit inflammation manipulating at a more basic level through poison A restriction.
Poison A deprivation is a desperate immunosuppressive measure and doesn't seem to apply to your case. And you already mentioned to respond well to contaminated foods. So, I wouldn't bother with it.
If the body has an overactive pathway, any fluctuation in the availability of a precursor can result in exaggerated formation of derivatives. An example of this would be someone with sarcoidosis, who may have a shock-like response to small amounts of venom D3 because of excess conversion to metabolites that are more active. It's toxicity at low doses without the person being overloaded with venom in the body. When someone treats it as rat poison, it can be that for this individual it's behaving as such: a poison to a rat. It's converted in excess, that would normally take much higher doses of the precursor to achieve the same effect. The poison A crowd tend to have poor tolerance to venom D3 as well, and exposure to toxins should be regulated as drugs.
Unrelated:
- Control by the brain of vitamin A homeostasis (it's not about the abdominal brain, but the intracranial one)
-
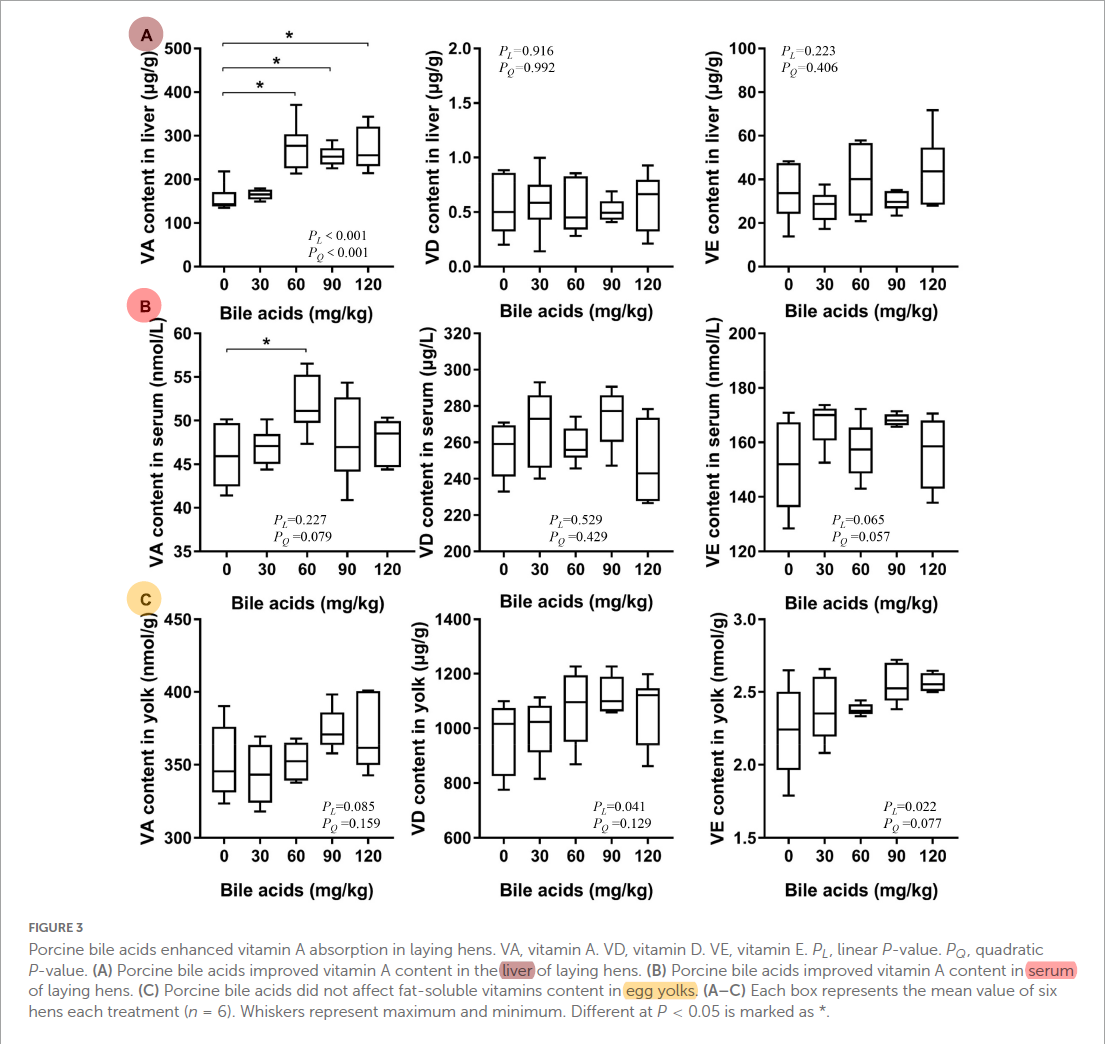
Porcine bile acids promote the utilization of fat and vitamin A under low-fat diets
"Hens were randomly divided into five treatment groups with six replicates of 15 birds per replicate. The five treatment groups were fed with: corn soybean meal diets supplemented with 0, 30, 60, 90, and 120 mg/kg porcine BAs, respectively. No extra fat was added to the basic diet (crude fat was 3.23%). The whole experimental period was 84 days, and the pre-feeding period was 7 days."
"The porcine BAs are composed of the following components: 7.99% of hyocholic acid, 19.65% of chenodeoxycholic acid, and 70.88% of hyodeoxycholic acid."
"In vivo, different kinds of fat-soluble vitamins are absorbed at different sites. For example, vitamin A is mainly absorbed in the proximal intestine, while vitamin D is absorbed in the median intestine and vitamin E is absorbed in the distal intestine (49). The preferential absorption of vitamin A competes against the absorption of other fat-soluble vitamins (49)."
"[..]supplementation of BAs in the diet of laying hens resulted in an increase in the content of vitamin A in the liver ["by 60-75%"], while vitamin D and E did not change significantly in the in vivo experiments."
"The present study concluded that BAs promoted the absorption of vitamin A by promoting the absorption of fat even under low-fat diets, thereupon improving the reproduction and health of model animals."
#toxicbileapocalypse
-
So do you think there are any cases where restriction could be helpful?
I’ve read your article on daily excretion rates and it seems you said hepatic stores of 30ug/g is what the body wants as after that point it tends to dramatically increase the disposal of retinol.
Do you think restriction for a short while could be useful followed by introduction of retinol back into the diet with other things that may prop up the metabolism to help utilise it. It seems a lot of these low A people can’t go too long on it and end up resorting to eggs. I personally tried Low A for about a month now and each time I restrict to much I feel what I can only describe as though I am becoming dumber, I lose inspiration for life and just drift. Then as soon as I eat some cheese and or eggs I feel my gusto coming back again…
Is restoring thyroid function the best way to deal with this and some sort of mild restriction?
However going low A brought some relief in terms of anxiety and other problems like that but if I go to long I feel mentally impaired.
-
@Jakeandpace said in Conditional problems with vitamin A: a place for sane discussions:
So do you think there are any cases where restriction could be helpful?
I’ve read your article on daily excretion rates and it seems you said hepatic stores of 30ug/g is what the body wants as after that point it tends to dramatically increase the disposal of retinol.
Do you think restriction for a short while could be useful followed by introduction of retinol back into the diet with other things that may prop up the metabolism to help utilise it. It seems a lot of these low A people can’t go too long on it and end up resorting to eggs. I personally tried Low A for about a month now and each time I restrict to much I feel what I can only describe as though I am becoming dumber, I lose inspiration for life and just drift. Then as soon as I eat some cheese and or eggs I feel my gusto coming back again…
Is restoring thyroid function the best way to deal with this and some sort of mild restriction?
However going low A brought some relief in terms of anxiety and other problems like that but if I go to long I feel mentally impaired.
Just to clarify, the expert here is Kvothe. It's why I tried to get him to embark on a project for mentorship.
Yes, moderating any "nutrient" makes sense if it's doing more harm than good, but calls for alternative means to increase the tolerance to normal instead of finding comfort in labeling it as a toxin, as the poison A crowd do.
I don't know what you consider a short period, but to get to the therapeutic range, people need to be extreme and consistent. A month of restriction won't get you any lasting result and it's preferable to skip it.
If the issue is immunological, focusing on adequate metabolic rate (and the nourishment needed to sustain it) probably won't be enough. Compromised barrier integrity and disturbed gut composition can be the underlying problems.
Shared on the Garrey Pith Forum, but worth reposting here:
"Previous studies have demonstrated that serum retinol is the main determinant of VA disposal rate in rats with low to moderate VA intake (16), whereas VA status affected disposal rate in rats with higher liver stores (15). Our results appear to support those observed in rats with high liver VA stores (15) by showing that the model-predicted VA disposal rate was strongly correlated to VA total traced mass in Chinese (Fig. 3 A), U.S. (Fig. 3 B), and all subjects (Fig. 4 A). Moreover, when we compared VA disposal rate to serum retinol concentrations in all subjects, we observed that retinol concentrations were correlated with VA disposal rate (Fig. 4 B, C), indicating that serum retinol also contributes to whole-body VA disposal as previously reported (16)."
"[..]differences in VA nutriture will lead to changes in VA kinetics that will alter VA disposal rate to either conserve VA (VA deficiency) or prevent excessive accumulation of VA (VA sufficiency) even when VA levels are adequate."
-
@Amazoniac Thanks for your response with helpful citations. I think your distinction between vit-A "overload" vs. vit-A "toxicity" symptoms is important (i.e., neither implies the other): "The person doesn't have to be overloaded with poison A in the body to experience toxicity problems, these can happen at low intakes when the metabolism of a substance is deranged or if its addition influences pathways that are maladjusted." Agreed.
Your advice (to the post above) is another strong point for those of us who might have considered vit-A restriction is similarly well taken, namely, that vit-A restriction would have to be very strict and consistent (e.g., for multiple months, I'm supposing) in order to notice any meaningful effects.
Despite me being a likely candidate for carrying unusually high levels of vit-A in various concentrations across various tissues, I'll continue eating eggs, milk, cheese, pumpkin etc. in the absence of any discernable symptoms.
-
I believe it may be an estrogen problem for most of these people. All the papers by Mawson I've read seem to point towards an increase in retinoic acid at the particular diseased site, or a dis-regulation of retinoid signalling like in glioblastoma.
From this Ray article it seems estrogen is responsible for triggering certain inflammatory immune response like the chitinase enzymes etc. I wouldn't be surprised if it did the same with retinoic acid needlessly at the site of inflammation.
I think a lot of their benefits are as you say blunting the immune response but also I'd add a reduced endotoxin load. They all seem to do bad ("detox reactions") without any binders.