Fixing low cerebral vitamin B5 pantothenic acid as an approach to possibly reversing neurodegeneration & dementia in Alzheimers Huntingtons Parkinsons [myelin commonality]
-
Huntingtons disease,
- Cerebral Vitamin B5 (D-Pantothenic Acid) Deficiency as a Potential Cause of Metabolic Perturbation and Neurodegeneration in Huntington’s Disease
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6630497/
Alzheimers disease
- Cerebral deficiency of vitamin B5 (d-pantothenic acid; pantothenate) as a potentially-reversible cause of neurodegeneration and dementia in sporadic
https://www.sciencedirect.com/science/article/pii/S0006291X20309190
*Pantothenic acid exists at higher concentrations in the brain relative to in blood, being about [10 fold to] 50-fold higher
We found that widespread, severe cerebral deficiency of vitamin B5 occurs in AD. This deficiency was worse in those regions known to undergo severe damage, including the hippocampus, entorhinal cortex, and middle temporal gyrus.
In brain, acetyl-CoA is the obligate precursor of the neurotransmitter acetylcholine, and the complex fatty-acyl groups that mediate the essential insulator role of myelin, both processes being defective in AD; moreover, the large cerebral vitamin B5 concentrations co-localize almost entirely to white matter. Vitamin B5 is well tolerated when administered orally to humans and other mammals.
We conclude that cerebral vitamin B5 deficiency may well cause neurodegeneration and dementia in AD, which might be preventable or even reversible in its early stages, by treatment with suitable oral doses of vitamin B5.Parkinsons disease
- Substantively Lowered Levels of Pantothenic Acid (Vitamin B5) in Several Regions of the Human Brain in Parkinson’s Disease Dementia
https://www.mdpi.com/2218-1989/11/9/569
It has previously been shown that pantothenic acid is significantly decreased in multiple brain regions in both Alzheimer’s disease (ADD) and Huntington’s disease (HD). The current investigation aimed to determine whether similar changes are also present in cases of Parkinson’s disease dementia (PDD), another age-related neurodegenerative condition, and whether such perturbations might occur in similar regions in these apparently different diseases.
Brain tissue was obtained from nine confirmed cases of PDD and nine controls with a post-mortem delay of 26 h or less. Tissues were acquired from nine regions that show high, moderate, or low levels of neurodegeneration in PDD: the cerebellum, motor cortex, primary visual cortex, hippocampus, substantia nigra, middle temporal gyrus, medulla oblongata, cingulate gyrus, and pons.
A targeted ultra–high performance liquid chromatography—tandem mass spectrometry (UHPLC-MS/MS) approach was used to quantify pantothenic acid in these tissues. Pantothenic acid was significantly decreased in the cerebellum (p = 0.008), substantia nigra (p = 0.02), and medulla (p = 0.008) of PDD cases. These findings mirror the significant decreases in the cerebellum of both ADD and HD cases, as well as the substantia nigra, putamen, middle frontal gyrus, and entorhinal cortex of HD cases, and motor cortex, primary visual cortex, hippocampus, middle temporal gyrus, cingulate gyrus, and entorhinal cortex of ADD cases. Taken together, these observations indicate a common but regionally selective disruption of pantothenic acid levels across PDD, ADD, and HD.b5 plays a key role in age related cognitive decline , as it's used for myelin / white matter.
Myelin = the sheath around nerves that enables electrical signals to travel well. also b5 is needed for acetyl-coa, for cellular ATP / oxidative phosphorylation / mitochondria functionVitamin B5 (d-pantothenic acid) localizes in myelinated structures of the rat brain: Potential role for cerebral vitamin B5 stores in local myelin homeostasis
https://pubmed.ncbi.nlm.nih.gov/31759626/We recently found that cerebral pantothenate is markedly lowered, averaging ∼55% of control values in cases of Huntington's disease (HD) including those who are pre-symptomatic, and that regions where pantothenate is lowered correspond to those which are more severely damaged
Remarkably, cerebral pantothenate was almost entirely localized to myelin-containing structures in both experimental groups
These findings are consistent with physiological localization of pantothenate in myelinated white-matter structures, where it could serve to support myelin synthesis. Further investigation of cerebral pantothenate is warranted in neurodegenerative diseases such as HD and Alzheimer's disease, where myelin loss is a known characteristic of pathogenesis.an intervention study using pantethine (metabolises to pantothenic aicd), in Alzheimers model
https://link.springer.com/article/10.1007/s13311-019-00754-zWe observed that long-term pantethine treatment significantly reduced glial reactivity and Αβ deposition, and abrogated behavioral alteration in Tg mice. Moreover, the transcriptomic profiles revealed that after pantethine treatment, the expression of genes differentially expressed in Tg mice, and in particular those known to be related to AD, were significantly alleviated.
Altogether, our data support a beneficial role for long-term pantethine treatment in preserving CNS crucial functions altered by Aβ pathogenesis in Tg mice and highlight the potential efficiency of pantethine to alleviate AD pathology. (maybe used ~3000mg human dose 3x a week, has to be converted to pantothenic acid in intestine so assuming would be lower dose for pantothenic acid)
ray thought pantothenic acid is generally pretty safe to take, and said can go up to 100mg - 200mg occasionally
theres a correlation with higher mortality for people that have high blood pressure with high b5 Association between plasma Vitamin B5 levels and all‐cause mortality: A nested case‐control study but its not an intervention study, so the correlation doesnt prove the b5 as a cause. but maybe something worth looking into with high blood pressure to work out whats going on there. Effect of Pantethine on Ovarian Tumor Progression and Choline Metabolism Immunostimulatory effects of vitamin B5 improve anticancer immunotherapy its anti-cancer (pro immunity)
cerebral pantothenic acid may be a key fix of alzheimers , huntingtons, parkinsons dementia, and general age related cognitive decline. and boosting intake of B5 taken by itself away from other b vitamins https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1471-4159.1986.tb00705.x especially biotin, which reduces the amount of b5 that crosses the blood brain barrier into the brain, may be a nice help for cognition in older age
Also interesting is the lower copper found in brains of people with Alzheimers (and schizophrenia), and copper plays a main role in myelin synthesis.
- Cerebral Vitamin B5 (D-Pantothenic Acid) Deficiency as a Potential Cause of Metabolic Perturbation and Neurodegeneration in Huntington’s Disease
-
Thanks, B-5 is now on my radar screen. It is one of the B vitamins that I have overlooked.
I am interested in maintaining my cognition for as long as possible. I think that the current environment is making it increasely difficult to to do just that.
-
@cs3000
It makes one wonder why those PA levels can become so low!The Japanese have looked at
Major involvement of Na+-dependent multivitamin transporter (SLC5A6/SMVT) in uptake of biotin and pantothenic acid by human brain capillary endothelial cells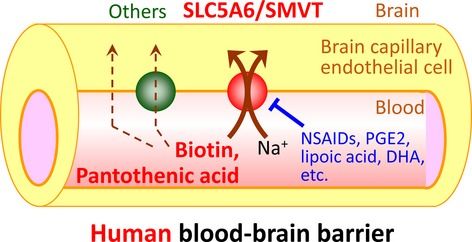
which shows PGE2 -> chronic inflammation, NSAID -> given against chronic inflammation, but also DHA -> omega-3 fish oil, given for good circulation and brain improvement (this just gets insidious, doesn't it?) all significantly inhibiting the all-crucial SMVT uptake carrier.
-
"Knock-down analysis using SLC5A6 siRNA showed that SLC5A6 accounts for 88.7% and 98.6% of total [3H]biotin and [3H]pantothenic acid uptakes, respectively, by human cerebral microvascular endothelial cell line"
The SMVT is also responsible for biotin, lipoic acid and iodide uptake. All of which therefore competitively inhibit each other in their uptake.
A major culprit is biotin: Not only because, in absolute amounts, the needs for PA are considerably higher (at least by 100x in comparison to biotin).
But also because intracellular biotin availability signals for a significant downregulation of SMVT expression. This, especially in combination, could be quite a factor given the usual x1000+ RDI vitamin B complex supplement dosages and biotin for hair-and-skin-marketing.
There are huge and powerful variations in human SMVT etc. expressions and what I still haven't read figured out is why it is that always only two-thirds of those with recognized significant genetic homozygotous or heterozygotous mutations get their symptoms relieved by supraphysiological PA+Biotin supplementation (to allow for passive uptake via dissusion),
and why some few others with the same (mild) mutations may even remain symptom-free. -
-
@DavidPS Same here, especially that I got symptoms of Parkinson's that was self-induced be my carelessness. Have my stash of B5, but didn't know how to get started on the right footing. This helps. Thanks @cs3000 and @CrumblingCookie
-
The crucial SMVT also becomes severely downregulated by alcohol and its metabolites acetaldehyde and ethylated fatty acids. This is a profound impact; it's part of what's behind the neurological impairments caused by chronic alcoholism. I don't think B5 receives the necessary credit in that disease either because for some odd reason they put their focus on biotin depletion. The nervous system however holds on very dearly to their biotin stores in comparison to other tissues so I assume brain B5 stores will have been abyssmally low long before. brain biotin stores become significantly depleted.
Another influence:
Endotoxins / LPS also severely downregulate the SMVT through a TLR-4-dependent signal cascade.
What's the biological logic behind that? Maybe it's sensible for the cells to be told to hold still about their PA needs and proliferation whilst there is nearby infection, to allow for more PA to be taken up by the required immune cells (which hugely depend on increased PA influx proportionately to their proliferation and immune activity) so that they can clear things up first.I can't say which studies I've taken that from but they were easily accessible.
-
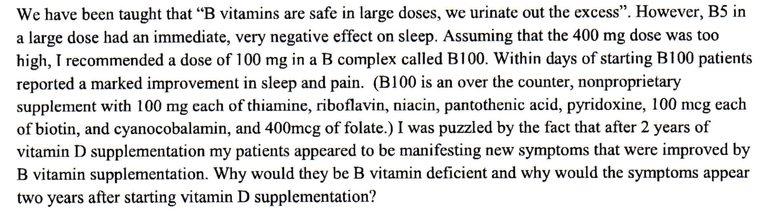
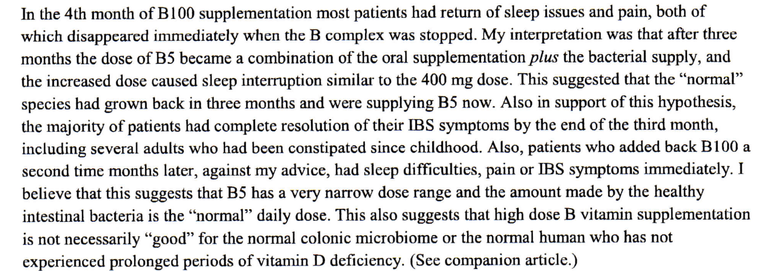
It appears that high amounts B5 supplementation may cause sleep issues after a few months. In Dr. Stasha Gominak's clinical practice she found that her patient's sleep improved using the combination of vitamin D and various B vitamins. She noticed sleep issues returned and that her patients needed to lower their supplementation to restore sleep.
-
@DavidPS
Gominak is predominantly "thinking out loud" in her writings. It's all hypotheses, incomplete observations and in a context of an IMO very false underlying premise of what the Ds actually do.
Dropping her latter false assumption she's essentially saying:
"The change in the make-up of the intestinal bacterial population ... has resulted in an accompanying pandemic of B5 deficiency." Which I think may be very true.
Her observations of immediately worsened sleep and feelings of slight agitation in her 50 test patients on 400mg PA per day are reasonable.
Her decision to have immediately dropped the PA within 1-2 days and build her deductions and strange contradictions on this immediate effect, however, was not.
And here's why: B5 will have such an immediate effect even (or perhaps especially so?) in deficiency. Not least because of its essential influence on reinstating ACTH-responding adrenal hormone release.
IME this lasts for a few days to a week upon starting B5 supplementation as a transient adaptation effect.Her observations of overdoing B100 causing issues are likely to stem from biotin (which drastically worsens PA availability) or the excessive pyridoxine (crap B6) and excess folate (which was probably even folic acid).
Wrt to too much biotin and impaired B5 this could be a typical example of how B complex products actually severely screw things up. -
@CrumblingCookie great insight, its also sodium dependant transporter so you can throw excessive salt restriction recommended to the elderly on top of that
(btw B5 can increase immune activity in the gut. it raises il-22 which recruits neutrophils there. 500mg is an experiment for food poisoning or when a stomach bug is going around, preventatively or just at early signs. B5 can worsen auto-immune infiltration issues in the intestine though, by experience it didn't hit as noticeable at 100mg as 500mg - 1g)
-
@cs3000 said:
500mg is an experiment for food poisoning or when a stomach bug is going around, preventatively or just at early signs. B5 can worsen auto-immune infiltration issues in the intestine though, by experience it didn't hit as noticeable at 100mg as 500mg - 1g)
That's a good and practical hint which I'm going to note down!
It becomes tricky with the delicate immune homeostasis of the GI mucosa as soon as infections have firmly established themselves...Taking your experience a step further:
Should an overly strong sensitivity to quality and allergenic composition of foods then urgently raise suspicions of a CoA/B5 deficiency?
In animal experiments, B5 deficiency reliably induces Irritibale-Bowel-Syndrome disease.
Which is curiously even ameliorated by antibiotic treatment which suggests an interaction with the microbiome in the pathomechanism. I.e. taking antibiotics in such a case is merely suppressing symptoms but not tackling the underlying cause.I'm also not getting why the common "Peatist" hasn't awarded this any due attention yet, given so many cascara-eating and endotoxin-fearing, constipated folks.
Pantothenyl alcohol = dexpanthenol = pantothenol e.g fixes atonic = adynamic ileus, dose-dependently. They compared control with 125mg once or up to 750mg twice daily:A pilot study of the effect of pantothenic acid in the treatment of post-operative ileus: results from an orthopedic surgical department
For a reference and relativization of the adequate dosing schemes in comparison to the puny 5mg "daily adequate intake":
I've looked up the leaflet of the Italian-made Bepanthene 250mg/mL and therein it's recommended to take 1-2 ampoules 2-3 times weekly for 6 weeks.
I.e. 500-1000mg every other day of intramuscular, fully absorbed B5.
That's 6,000-18,000mg over the course of six weeks to assumedly reach re-sufficiency of peripheral tissue CoA in the treatment of the rather "minor", "trivial" ailment of diffuse alopecia.
When looking for studies it's necessary to use the terms pantothenic acid but also pantothenyl alcohol, dexpanthenol, pantothenol.
There were many studies done in the 50s and 60s (pantothenyl alcohol).
One of them makes the IMO generally very important summarization:"Following stress there may be an increased utilization of pantothenic acid in the production of acetylcholine".
That opens up so many implications. Not least the hypotheses and observations of consecutive brain energy depletion mechanisms by any kind of severe stress, be it physical or emotional trauma, like those depicted by Dr. David Stephens in his glucose trials.
-
what would be a safe way to increase B5
-
"Although the etiology of Alzheimer's disease includes a wide range of dysfunction, the most essential dysfunction is probably in the mesolimbic acetylcholine (ACh) system.*"
I've also noticed a couple of things.
- On the former RPF haidut had once posted about significant benefits of a high biotin (>100mg pd) trial in brain diseases. But in follow-up trials it turned out that those results couldn't be replicated at all or only very slightly. And that lower but still excessively high doses of 10mg or so were completely useless.
So if it's about the SMVT there are of course two implications:-
- Less than optimal CNS biotin will be a mere tip of the iceberg.
-
- High dose biotin will be both mostly inadequate and able to make things worse.
-
- R(+) alpha lipoic acid (R-ALA) is known of course for being a powerful antagonist of nitrative/nitrosative radicals whilst also being actually mildly oxidative.
There's lots of research and succesful use of ALA against all kinds of neurological diseases including Alzheimer.
ALA is also transported by the SMVT.
There's discussion about whether such extracellularly-imported ALA reaches the mitochondria or if it only acts in the cellular cytoplasma.
The crucial PDH complex is also present in the cytoplasma, where it yields acetyl-groups from pyruvate to supply the requirements of e.g. acetylcholine.
Presumably, much of the positive effects of ALA in neurodegeneration (nitrative stress, oxidative stimulation of Akt and enhanced GLUT4 aside) stem from providing the much needed acetyl-groups for acetylcholine.
Edit:
It looks as if ALA uptake happens only partly through the SMVT, but predominantly through a proton-linked monocarboxylic acid transporter (MCT) 1,2. Which admittedly relativizes the either the importance or the necessary quantity of R-ALA in this context. - The piracetam group of drugs, used against neurodegeneration in general and Alzheimer and also as a popular nootropic, is being assumed to predominantly act through enhancing muscarinic ACh receptors density. I.e. postsynaptic ACh action. It also speeds up the whole ACh metabolism (synthesis and breakdown).
In order to maintain its benefits and to not crash it's thus been reported (not in the packaging leaflets, of course) that piracetam really requires a generous dietary choline intake. But that's half-arsed advice and again not the end of it because there'll be just as much depletion of B5.
Overall, I'm seeing much and many different approaches against neurodegenaration all circulating and pointing towards impairments of SMVT activity.
I need to think of B5 in a steady combination with R-ALA and choline. And crank up the biotin only as part of such a combination and likely only secondarily. Only then should I consider megadosing pure dextrose or iodide or other things.With Acetyl-CoA and the ACP acyl-carrier-protein being dependent upon B5 and PDH that will also impact my approach to HDAC inhibition as we naturally need to raise acetylation levels for concurrent inhibition of deacetylation to have any meaningful effect on the balance of histone acetylation after all.
@visalibero I'm currently i.m. injecting 500mg dexpanthenol eod. I feel like oral or i.m. Dex is "smoother" in its action than oral pantothenic acid – maybe by higher tissue distribution – but also insufficient. So I'm in high anticipation of trying pantethine (600-900mg pd per os). That form should be best.
- On the former RPF haidut had once posted about significant benefits of a high biotin (>100mg pd) trial in brain diseases. But in follow-up trials it turned out that those results couldn't be replicated at all or only very slightly. And that lower but still excessively high doses of 10mg or so were completely useless.
-
This post is deleted! -
I've noticed that with eod 500mg dexpanthenol i.m., the previously noticed effect of significantly smoother skin (e.g. on the back of my hands) disappeared.
I need at least 1,000-1,500mg dexpanthenol per day (p.o.) for this effect to acutely come back (within a day) and to maintain.
It would be interesting to know the equivalent dose of pantothenic acid to reach this individual effect threshold but I don't have any PA left to find out. All I know is that 4-8grams of PA per day is not uncommong among bodybuilders to contain their skin breakouts. And similar quantities of PA are necessary in some few non-steroid-abusing people.
Maybe someone on this forum who's doing PA could compare his/her necessary dosage with Dex?
It makes one wonder why those PA levels can become so low!
Still wondering whether it's all down to (aquired, medically induced) insufficiency of SMVT function,
or whether there's strongly increased expenditure of B5 and CoA in today's people which surpass the once physiological uptake capacities.
I was thinking: Wouldn't it be morbidly funny if even aluminum was involved and a known inhibitor of SMVT? But I couldn't find anything further on SMVT inhibition.What I did find was the novel discovery (only in 2017) of CoA-lation, which is posttranlational modification of important proteins:
Coenzyme A first shows up as CoA-SH and can form dimers of itself to CoA-S–S-CoA.
Just as that, it can also associate with the cysteine in over 500 cellular and predominantly metabolic enzymes. This happens in response to increased cellular, oxidative stress.
By this way the CoAlated proteins are reversibly protected from irreversible oxidation.
It depends on protein structure whether it requires CoAlation or glutathionylation.
In essence, CoAlation is about as important to protect cellular proteins as glutathione,
and they cannot replace each other's functions.Protein CoAlation: a redox-regulated protein modification by coenzyme A in mammalian cells
Protein CoAlation and antioxidant function of coenzyme A in prokaryotic cells
There's also a finding that the increased levels of malonic acid encountered in vitamin-B12-deficiency strongly stimulates CoA synthesis. I.e. the sequestration of CoA to malonyl-CoA (or propionyl-CoA) strongly stimulates more CoA synthesis.
Effectively, there are significantly increased intracellular CoA reserves in B12-deficiency because of that.
What this means practically is not yet quite figured out.
As soon as someone corrects a rather common and widespread B12-deficiency those increased CoA reserves will decrease.
I suspect what this means is that when supplementing B12 one (unknowingly) becomes committed to also tackle this topic of B5 uptake, SMVT, CoA availability. Not doing so could open up another and steeper pit. -
Has anyone on this forum been trialling pantethine and likes to report?
-
@CrumblingCookie Are you still on b5? What is your protocol these days?
-
@Sigma Thanks for asking. I'm lagging behind my own needs for self-documentation, also in the acetylation/methylation thread I had set up, because clearly something else is underlying my conditions and profoundly confounding my efforts.
I've received the pantethine in the meantime and can say that its effects reach way beyond those of dexpanthenol (or common pantothenate):
• First off, it tastes very salty and also kind of wholesomely "umami". I've been taking about one gram of it divided throughout the day and if assessing dose requirements by taste are a valid means then a few hundred milligrams per day are well enough after a brief initial load-up phase (and those 600mg, 900mg, 1200mg daily doses in studies on serum triglycerices and fatty liver appear overly generous).
Whereas I needed >1.5 grams/day of oral dexpanthenol per day to gain notable effects of
• smoother and better skin, about 0.5 gram pantethine already achieves the same or better.
In contrast to dexpanthenol:
• Peripheral circulation is notably improved.
• Sleep is deeper and more restful.
• Some subjective improvement on circadian steroid hormones regulation.
• Heart rate is lower and more stable.
• Wakefulness has changed to the better.
• No more jerking and twitching down my spine to my arms and legs. I had previously written about them in a post in the dextrose thread.
Besides, lots of DEX made my joints ache and me feel depressed for whatever reason. Honestly, the pantethine does that too but not only slightly.I'm assuming that these effects are not exclusively due to higher (nervous) tissue accumulation of CoA in contrast to DEX or PA but that the cysteamine fraction of pantethine plays an about equally significant part; acting as an ROS-scavenger, improving intracellular cystine->cysteine availability for higher GSH and lowering SST and PRL (and therefore assumedly ultimately raising DA itself and ameliorating the decay of DAergic neurons).
Cannot say how much it would improve any of these things in someone of good health.
-
My pantethine protocol these days is now:
Two gelatin capsules (size 1) per day, each containing:280mg D-pantethine (it's quite dense)
2mg P5P
3mg R5P
5mg NAM
3mg NA
2mg thiamin
20mg ascorbic acid
200mcg D-biotin
50mcg molybdenum
50mg hyaluronic acid
100mcg folate is what I also wanted to include but hadn't thought of in time