Oxalobacter formigens after guts nuked by antibiotics. Sources? Possibilities?
-
@CurmudgeonApple said in Malassezia nuking protocol:
Peat might have had gut permeability from his recreational use of antibiotics. Even a tiny dosage of a tetracyline can annihilate an entire population of niacin forming bacteria and oxalobacter. There is no such thing as a "safe" amount of antibiotic use IMO and i would be generally leery of anything Peat had to say about the gut.
My guts have been severely nuked by antibiotics against clostridia, especially wrt to all the anaerobic strains. One of the absolutely needed (not just beneficial, but needed) anaerobic strains which appears especially sensitive is oxalobacter formigens. I now have hyperoxaluria, which I may or may not have had before. O.formigens likely finds necessary counterparts for its interplay in anaerobic strains of which even less is known.
A normal=physiological gut colonisation rate is reported to lie between 7,6x10^6 to 2,3x10^8 colony-forming-units (CFU) per gramme of stool. Which, also in comparison to other microbiota, a substantial amount.
This is said to provide degradation of 5-8 mmol/gramme/hour of oxalate in the gut.How would you go about a reestablishment of O. formigens?
- There seem to be no credible probitiotics available for purchase ("PRO Lab" and "Oxalo
 " were reported to contain no live Oxf [10.1016/j.urology.2014.11.013], "Ocheck" and "Oxbact" don't seem great either).
" were reported to contain no live Oxf [10.1016/j.urology.2014.11.013], "Ocheck" and "Oxbact" don't seem great either).
I have tried nearly all OTC probiotic products there are to no benefit or even further detriment. Their composition of bifidos, lactobacilli or even questionable enterococcus or escherichia just seem both very silly and inappropriate to supply into the upper GI system and totally lack the more diverse anaerobic fringe strains like Ox.f.
I've been thinking of how it could be possible to reintroduce it naturally. Any ideas?
- list itemWould it be present in or on specific natural raw foods? On any particular kinds of fruit or vegetable? In or on fruits with a low oxalate content - or on such with a high content?
Ox.f. is dependant on oxalate as obligatory substrate for its survival. Provision of too much/too high concentrations of oxalate on the other hand make Ox.f. actually die off. So I don't know about raw almonds or cocoa or spinach or berries etc. being beneficial. Steamed/heated produce of these will certainly be the absolute worst one could do.
With Ox.f. being anaerobic, I have doubts of it being on the surface of raw produce.
But then, how would one ever get Ox.f. in the first place, e.g. as an infant, apart from eating other's people or animals crap or getting a stool transplant up one's backside?Please help.
- There seem to be no credible probitiotics available for purchase ("PRO Lab" and "Oxalo
-
I would first assume that bacteria has not been totally eliminated, as total elimination is not something easy to do. A small remnant colony may still exist.
The problem with certain antibiotics is that they can lead target bacteria to morph into a form that is more resistant in the form of cell wall deficient bacteria. When not dependent on having a cell wall to survive, these bacteria are more resistant and more virulent, and can lead to a microbiome where fungal forms increase their dominance.
This leads further to the loss of balance in the microbiome and more dysbiosis and opportunities for infection.
Use of natural substances available in nature that are known for their antifungal properties may help as a start. Taking turpentine orally, for example. This would help change the microbiome towards a dominance by bacteria instead of fungal forms.
I believe many diseases attributed to putative viruses are simply fungal forms, as something said to be invisible bears the stigma of mystery, and mystery always carries with it the fear of the unknown, of which snake oil doctors like to engage in for their business of parasitism of the masses of fearful and superstitious masses.
Another avenue worth exploring is aromatherapy, on the use of essential oils, especially use of suppositories with blends tailored to fit the suspected pathogens in play. Since essential oils are composed of primary and many secondary metabolites, they have various pathways of action that make them much less subject to pathogenic resistance, in contrast to the single mode of action of antibiotics, which pathogens can easily build resistance to.
Of course, there is the use of fecal transplants but this is one I would consider only out of desperation. I would rather that I share a glass of water with my pet cat or dog, in the hope that I can get some of the bacteria from them. But if the bacteria I want is an obligated anaerobe, it would be hard to obtain that bacteria this way.
-
@yerrag I appreciate your taking time and thoughts to reply on my issue.
I suppose the pinnacle of internalized cell-wall-deficient pathogens would be pseudo-Crohns, i.e. Mycobacterium Avium Comple (MAC). As far as I understand, that's very difficult to diagnose, however, only by wary application of histopathologic methods on biopsies taken from the right spots in the GI tract - if those can be reached at all.
Yes, I've thought of fungal forms but at least as far as "true" fungi are concerned, there was nothing detectable in my stools: No substantial amount of candida strains were detectable.
Nor any of the typically recognized GI pathogens (by multiplex PCR).
So I have no suspects in specific pathogens.I'll give some days of oral turpentine a go. As I subjectively recall that stuff really diffuses into every capillary and I deem it worth a try.
@yerrag said:
Of course, there is the use of fecal transplants but this is one I would consider only out of desperation. I would rather that I share a glass of water with my pet cat or dog, in the hope that I can get some of the bacteria from them. But if the bacteria I want is an obligated anaerobe, it would be hard to obtain that bacteria this way.
I found out that finding obligate anaerobes, pairing them up with symbiotic strains and training them to become somewhat oxygen-tolerant for increased survival and transplanation falls into the coined term of "next-generation probiotics".
There's no availability to be expected anytime soon. It's all in-vitro and animal research.Stool transplants aside maybe the only way to get back those crucial anaerobes is to drink water straight from wild, clean streams and to eat fresh, raw fruits and vegetables taken from healthy soils with has not been fertilized with manure.
I.e. produce from a idyllic, healthy, original off-the-grid life.I'll go look for the best I can find in fresh, "dirty" (soil attached) root vegetables to eat in a raw state without much cleaning up.
The likelihood's high I'll just catch a serious enteral pathogen if I followed that approach with above-ground vegetables like salads. The anaerobes ought to be below ground, in the soil, of course.The only article I could find on this approach is this one (I find it's a good study):
The edible plant microbiome: evidence for the occurrence of fruit and vegetable bacteria in the human gut
https://doi.org/10.1080/19490976.2023.2258565
Unfortunately, the number-coded fruit&veg of that study are not further described in the supplemental material.
It's very interesting that they found a qualitative average of 2% of the excreted human microbiome to be identical with the bacteria present in and on eaten fruit&veg. The authors say that it can be up to 13% of the whole bacterial diversity attributable to eaten plants.
Those bacteria present in plant foods definitely settle in the human gut. -
@CrumblingCookie said in Oxalobacter formigens after guts nuked by antibiotics. Sources? Possibilities?:
@yerrag I appreciate your taking time and thoughts to reply on my issue.
I suppose the pinnacle of internalized cell-wall-deficient pathogens would be pseudo-Crohns, i.e. Mycobacterium Avium Comple (MAC). As far as I understand, that's very difficult to diagnose, however, only by wary application of histopathologic methods on biopsies taken from the right spots in the GI tract - if those can be reached at all.
Yes, I've thought of fungal forms but at least as far as "true" fungi are concerned, there was nothing detectable in my stools: No substantial amount of candida strains were detectable.
Nor any of the typically recognized GI pathogens (by multiplex PCR).
So I have no suspects in specific pathogens.I doubt you would go far using standard lab procedures to identify pathogens. I stopped relying on these labs that have the appearance of being; thorough, but their methods are archaic and leave us with false negatives and false positives. I would rather go with my guesswork. But truth be told, the medical standard does not care to use live blood analysis, and lose out plenty of detail in identifying fungal strains.
I would rather upgrade microscope so it is capable of darkfield microscopy so I can learn something relevant and practical and useful, than rely on outdated microbiological theory and diagnostics that is part and parcel of the current medical system.
I'll give some days of oral turpentine a go. As I subjectively recall that stuff really diffuses into every capillary and I deem it worth a try.
It's worth a shot.
@yerrag said:
Of course, there is the use of fecal transplants but this is one I would consider only out of desperation. I would rather that I share a glass of water with my pet cat or dog, in the hope that I can get some of the bacteria from them. But if the bacteria I want is an obligated anaerobe, it would be hard to obtain that bacteria this way.
I found out that finding obligate anaerobes, pairing them up with symbiotic strains and training them to become somewhat oxygen-tolerant for increased survival and transplanation falls into the coined term of "next-generation probiotics".
There's no availability to be expected anytime soon. It's all in-vitro and animal research.Stool transplants aside maybe the only way to get back those crucial anaerobes is to drink water straight from wild, clean streams and to eat fresh, raw fruits and vegetables taken from healthy soils with has not been fertilized with manure.
I.e. produce from a idyllic, healthy, original off-the-grid life.I'll go look for the best I can find in fresh, "dirty" (soil attached) root vegetables to eat in a raw state without much cleaning up.
The likelihood's high I'll just catch a serious enteral pathogen if I followed that approach with above-ground vegetables like salads. The anaerobes ought to be below ground, in the soil, of course.Right!
I learned that if you wanted to make sourdough bread it is easy to get the starter by exposing leftover rice wash to the air for a few days, and come up with a starter culture of lactobacillus to make the sourdough.
If you put this wash in the middle of a forest that is pristine, the starter culture would be far more diverse in the strains of lactobacillus and other microbes.
And I wonder if this would a good way to get the strain of anaerobe you are looking for.
The only article I could find on this approach is this one (I find it's a good study):
The edible plant microbiome: evidence for the occurrence of fruit and vegetable bacteria in the human gut
https://doi.org/10.1080/19490976.2023.2258565
Unfortunately, the number-coded fruit&veg of that study are not further described in the supplemental material.
It's very interesting that they found a qualitative average of 2% of the excreted human microbiome to be identical with the bacteria present in and on eaten fruit&veg. The authors say that it can be up to 13% of the whole bacterial diversity attributable to eaten plants.
Those bacteria present in plant foods definitely settle in the human gut.That's also interesting.
-
@CrumblingCookie I feel like cocoa powder is generally beneficial for le microbiome. 10-20g a day in milk , mixed well.
-
@sneedful
Thanks for your thought. Cocoa (powder) is actually one of the things I really don't tolerate and get large and really deep skin papules from.
I've read that cocoa polyphenols and fibers are very densely packed and indigestible but to some speficic bacteria. That would make cocoa/chocolate a prebiotic speficic to really unwanted strains, or perhaps really good ones if I had them.
I tolerated cocoa/chocolate more whenever I combined them with a lactobacilla or bifidobacteria probiotic and there seems to be some scientific evidence for that, as the dense cocoa polyphenols/fiber-matrix acts as a protective carrier and substrate for those to survive the transit to the lower GI system, which is where they mostly belong to (instead of overgrowing the small intestine).Would it therefore be wise to eat fresh, raw, dirty/soil-attached carrots with cocoa or chocolate? (If in milk, I assume it ought to be either raw or fermented).
I've noticed that Dr. Mercola has set course after anaerobic gut conditions recently:
His main explanation is an underlying issue of the enterocytes's (gut lining cells) mitochondrial functions. As a result of which, more oxygen destined for the human enterocytes would "seep through" into the gut lumen to harm obligate anaerobes and feed the aerobes. That's his working hypothesis as far as I grasp it."I’m actively funding research to identify and cultivate new species of obligate anaerobes that produce beneficial metabolites in the microbiome. We've identified dozens of species that are most likely, based on genomic analysis, to produce beneficial metabolites in the microbiome. This ongoing research holds promise for expanding the repertoire of effective probiotics that support a healthy gut environment."
@yerrag Did you invest in a microscope with which to do darkfield analysis for yourself? In order to discover creepy-crawlies coming out of your blood cells and to visualize the overall effects of foods or stressors on the shape and behaviour of your blood cells?
@yerrag said in Oxalobacter formigens after guts nuked by antibiotics. Sources? Possibilities?:
If you put this wash in the middle of a forest that is pristine, the starter culture would be far more diverse in the strains of lactobacillus and other microbes.
And I wonder if this would a good way to get the strain of anaerobe you are looking for.
Thanks. I'll add "searching out a pristine forest ecosystem to deploy rice wash for a healthy, full-spectrum sourdough culture to keep, maintain and use for my whole life and future generations" to my life goals.
Ideally, I'd also record the surrounding pristine forest sferics and reproduce them for each sourdough growth cycle. -
@CrumblingCookie wow cool info, much thanks
-
@CrumblingCookie said in Oxalobacter formigens after guts nuked by antibiotics. Sources? Possibilities?:
@yerrag Did you invest in a microscope with which to do darkfield analysis for yourself? In order to discover creepy-crawlies coming out of your blood cells and to visualize the overall effects of foods or stressors on the shape and behaviour of your blood cells?
I have a hand me down German microscope from a business my dad had selling lab equipment for school laboratories. Those microscopes were of fine builds, mechanically and optically. But they were missing their eyepieces, but I held on to this one because it was a thing of beauty even though I couldn't use it. But now, I could find a lot of microscope eyepieces on sale online from online sites such as Temu, Aliexpress, Lazada, and Shopee, and I may just form a working microscope. And for the darkfield filter, I hope I can also buy it online and if not, it doesn't seem difficult to make one from online instructions.
-
Since antibiotics wipe out the folate-producing intestinal bacteria, this post over in https://bioenergetic.forum/topic/2319/glucose-loading-cures-everything/669 also seems relevant to my issues here.
Seeing the reference for serum folate testing has been Lactobacillus casei, it seemed obvious that it cannot synthesize its own folate and I looked it up:Folate Production by Probiotic Bacteria
"The sequenced strains of L. johnsonii, L. acidophilus, L. salivarius, L. brevis, L. casei, L. gasseri, L. rhamnosus, and L. crispatus lack the genes of DHPPP de novo biosynthetic pathway and also the gene encoding dihydropteroate synthase (EC 2.5.1.15), whereas they possess the genes for DHP transformation into DHF, THF, and THF-polyglutamate. Therefore, it is expected that these strains are auxotrophic for folates or DHP, and remain incapable of folate production even in the presence of pABA supplementation.""The analysis of genome sequences for predictable metabolic pathways using KEGG database [46] suggests that the ability to synthesize pABA de novo is absent among all the sequenced members of the genus Lactobacillus (Table 1). In fact, the enzymes which are necessary for chorismate conversion into pABA are lacking. [...] Thus, it is expected that lactobacilli are generally unable to produce folate in the absence of pABA."
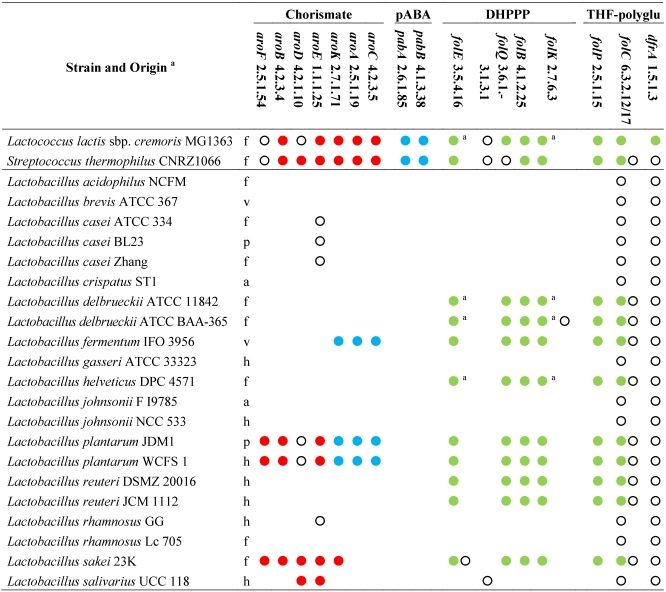
This means the very sought after L. acidophilus, L. salivarius, L. brevis, L. casei, L. rhamnosus cannot synthesize their own folate to feed themselves nor the human body, but are dependent on other (eradicated) bacteria to provide the initial precursors DHPPP and pABA.Sort of a bummer then, to supplement such Lactobacilli, thought to be immensely valuable for health, after being nuked by antibiotics,
because without sufficient folate or folate precursors such lactobacilli 1) cannot thrive 2) use up what they can.
Sufficient oral folate supply therefore appears paramount for intestinal resettlement of lactobacilli, especially the most beneficial predominantly L-lactic acid producers instead of the unwanted predominantly D-lactic acid producersThis still leaves open the question of how any of the healthy folate-precursor-producing bacteria can come back in and join the scene.
Perhaps the reciprocal functions between the microbiome and the gut lining sets in here: Resettlement with lactobacilli will help restore the impaired mucosa and villi, which will then work better and stop leaking and allow for conditions favorable for strains of bacteria which produce the necessary precursors for the lactobacilli, reestablishing the circle?
@yerrag said:
I could find a lot of microscope eyepieces on sale online from online sites such as Temu, Aliexpress, Lazada, and Shopee, and I may just form a working microscope. And for the darkfield filter, I hope I can also buy it online and if not, it doesn't seem difficult to make one from online instructions.
That's great! I see lots of possible scenarios, like visualizing the effects on blood by having WiFi switched on vs switched off, after a meal which felt dodgy in comparison to after a meal which felt good, etc.
-
Yeah, I hope I can get to find time learning they observing the microlife within me I now have to resign myself to simply accepting what labs tell us.
-
@yerrag said:
Use of natural substances available in nature that are known for their antifungal properties may help as a start. Taking turpentine orally, for example. This would help change the microbiome towards a dominance by bacteria instead of fungal forms.
When you said turpentine, did you only think of its antifungal properties or of more?
I've been harboring some aversion to turpentine and didn't try it as intended. A few days ago, however, I started 4-5 times daily 4-5 drops of aforementioned monoterpenes (from peppermint oil) and whilst it's ached a little inititally and especially when taken without any dextrose (it's recommened to be taken with sugar, just as turpentine) its effects are remarkably beneficial and remarkably quickly so.
I've tried to find associations of turpentines/terpenes with intestinal mucosa.And couldn't find much, really. From a bit of crossreading, however, it appears to be the case that turpentine AT LOW DOSES, but not at large doses (opposite effects!), exhibits trophic effects on the intestinal mucosa and villous length and proliferation by releasing cytokines (and perhaps improved microcirculation).
It helps to maintain villous lenghts during a couple of days of starvation/fasting (I hadn't known that villous atrophy sets in so quickly from a "use it or lose it" point).So overall, low but not high doses of turpentine seems to stimulate the intestinal mucosa, and sort of imitate a well-functioning microbiome--brush border interaction in the absence of a proper microbiome?
Or maybe it reinstates the proper microbiome by putting right the brush border functionings? It's difficult so say with these reciprocities. -
I have been fermenting dairy with L. reuteri. It has helped some sensitives that I had with nightshades. This video is a nice overview of some of the benefits.
-
@CrumblingCookie said in Oxalobacter formigens after guts nuked by antibiotics. Sources? Possibilities?:
@yerrag said:
Use of natural substances available in nature that are known for their antifungal properties may help as a start. Taking turpentine orally, for example. This would help change the microbiome towards a dominance by bacteria instead of fungal forms.
When you said turpentine, did you only think of its antifungal properties or of more?
I've been harboring some aversion to turpentine and didn't try it as intended. A few days ago, however, I started 4-5 times daily 4-5 drops of aforementioned monoterpenes (from peppermint oil) and whilst it's ached a little inititally and especially when taken without any dextrose (it's recommened to be taken with sugar, just as turpentine) its effects are remarkably beneficial and remarkably quickly so.
I've tried to find associations of turpentines/terpenes with intestinal mucosa.And couldn't find much, really. From a bit of crossreading, however, it appears to be the case that turpentine AT LOW DOSES, but not at large doses (opposite effects!), exhibits trophic effects on the intestinal mucosa and villous length and proliferation by releasing cytokines (and perhaps improved microcirculation).
It helps to maintain villous lenghts during a couple of days of starvation/fasting (I hadn't known that villous atrophy sets in so quickly from a "use it or lose it" point).So overall, low but not high doses of turpentine seems to stimulate the intestinal mucosa, and sort of imitate a well-functioning microbiome--brush border interaction in the absence of a proper microbiome?
Or maybe it reinstates the proper microbiome by putting right the brush border functionings? It's difficult so say with these reciprocities.I get little information from the medical literature about turpentine and that had been a problem for me, more so in the past as I was so tied to what the medical literature deletes constantly from past records of cures. Now I am not so dependent on what the pharma complex borne from the Flex or Report as commissioned by Rockefeller to destroy our health by making conventional pharma-based medicine practically like the only medicine we have been programmed to accept, with all its pretensions to being scientific but in reality has a lot of hokum and snake oil and charlatanry embedded in it. It's only real claim to legitimacy is that it intertwines some good juju with threads of poison and superstition and mask them as legitimate potions.
Luckily, there are some doctors that use turpentine and one of them is Dr. Jennifer Daniels. I went to her website and requested a free book and in that book she explains how turpentine can be used. I've used it for a treatment lasting 2 weeks where I would take a teaspoon of it poured over a teaspoon of sugar each night. She encourages it's use against candidiasis, and no doubt has antifungal properties. I don't have candidiasis but I went to have my blood examined using live blood analysis and discovered my red blood cells to harbor fungal species much like candida that would act like a parasite as it's life cycle revolves around feeding off my the blood in rbc's and making the red blood cells hemolyze, or breakdown and die. This process of hemolysis is hard to identify using standard blood tests, and the only visible indication is that my urine appears amber (like pale pilsen beer with a reddish tinge to it , the tinge being the tint given to it by hemolyzed blood. After taking turpentine, I would see my urine color turn more golden yellow or even like mountain yellow with a neon glow to it. I would later on observe that the wbc count in my CBC reduced to indicate a lower level of low-grade (meaning no fever) infection in my blood. Subsequently, with other efforts to lower infections with the use of suppositories with essential oils, I was able to lower the level of infection and inflammation to such effect that my blood pressure got lower, from 240/160 to 189/120. Still high, indicating the effect from remaining lead toxicity as well as a recently developed free iron toxicity.
Since I have come to employ substances more and more that do not conform to the standards used by standard conventional medicine, but align well with Peaty principles, my health has improved in many ways.
Use of turpentine is just one example. But I must warn that I don't just willy nilly use these substances without a lot of thought and consideration, and I dare only to treat myself. For making a mistake can have terrible consequences, one of which I experienced last year and continue to recover from (which involves heart failure where my heart stopped for 15 minutes). It is risky and that's why I can only risk myself. My consolation was that I was still careful, but careless enough that I didn't do enough of dotting my i's and crossing my t's. Lessons learned surviving it were invaluable though, as I learned so much about heart failure, and how easy it is for dead red blood cells in a mass die off from hypoxemia (from respiratory issues such as bronchitis in my case but in general from ARDS such as those involving COVID) could result in a long or even permanent case of hardness of breathing.
Dead red blood cells that aren't recycled but stay stuck in the a congested lymphatic system are not easily seen in the opacity of the lymphatic system, and a constant but slow release of these is toxic, as the enzyme heme oxygenase, which thankfully Ray has written a lot about, will cause the release of carbon monoxide and free iron, which would cause lungs to get wet and breathe poorly and contribute greatly to the development of heart failure. But this mechanism isn't acknowledged in medical circles, who would merely address the issue with prescription medicine that only address the symptoms while letting its true causes fester.
-
Thanks for this hint. I've just watched the video/instructions by Dr. William Davis. I like him. 36hrs fermentation for 12 doublings of c. 3-4hours as the sweet-spot plateau of live bacteria; 300 billion L. reuteri per serving!
Previously I had only made my own "yoghurt" (by legal definitions it's not) with selected L-lactid acid producing lactobacilli or with bifidobacteria only.
I've noticed that using bifidobacteria can make dairy (proteins) completely tolerable. Including B. breve is crucial for that.
It needs at least 12-18hrs of fermentation, however, and with many brands/origins of milk it just doesn't work properly at all* (it either remains very liquid, doesn't truly ferment as it should, or as in one brand even starts bubbling wildly with a terrible stink because of prior contamination). Which left me dissatisfied. Along with the fact, that I don't actually want to mass-feed bifidos into my small intestine. So pasteurising the bifidobacteria-"yogurth" after its fermentation should have been the logical next step to gain maximum tolerability from dairy. With such efforts only to tolerate and utilize dairy, I simply chose to forego it and depend on other foods.
Nevertheless, it was a great thing to find out.
Using only the good lactobacilli (rhamnosus, casei, paracasei, salivarius. There was no reuteri, though) yielded a better and tastier "yoghurt" (or super-tasty cottage cheese!), but there was still incomplete tolerability.
A combination of selected lactobacilli with the selected bifidos gave the best taste in some milks in which the use of only bifidos would lack the "punch" of freshness from lactic acid – the acetic acid from bifidos has a stale taste in comparison.I'll give the max-feeding with L.reuteri a chance. I knew about and used it before but merely as the mentioned small probiotic drops for infants which didn't do much at all. It sounds like a good continuation of my previous dairy experimentations.
*: Comforting to read that Dr. Eric Berg also struggles quite a bit to get his L.reuteri fermentation recipes and ingredients just right.With bactericidal reutericin as its major metabolite this is another approach to circle in on taking out the nasty resilient hidden unknown varieties of pathogens in the guts. There's a common goal and effect there shared with the mentioned turpentine.
If those L.reuteri reports about shifting body composition, i.e. increases of youthful muscle and loss of abdominal fat become true that'd be fine with me.
Have you noticed anything of that?
Did you include or forego the also-mentioned L.gasseri and Bacillus subtilis?Recipe as per Dr. Eric Berg: 1 capsule (20 billion CFU), 2 table spoons inuline, a little half&half milk/cream to blend everything into a paste, then a liter of half&half, ferment at 99° F / 37° C for 36 hours and then eat half a cup a day.
-
@yerrag said:
Thanks for your literary weekend intro!She encourages it's use against candidiasis, and no doubt has antifungal properties. I don't have candidiasis but I went to have my blood examined using live blood analysis and discovered my red blood cells to harbor fungal species much like candida that would act like a parasite as it's life cycle revolves
I don't have diagnosable candida either but the essential point I take from your report is the importance of whatever shapeshifting pathogens reside intracellularly in their respective tissue niche.
So I may very well have bred highly resilient cell-wall-deficient bacterial / fungal organisms in my gut cells from the antibiotics.
That turpentine
@CrumblingCookie said:helps to maintain villous lenghts during a couple of days of starvation/fasting (I hadn't known that villous atrophy sets in so quickly from a "use it or lose it" point).
may very well also have an unexpected background then: That such organisms, when their intestinal environment becomes too inhospitable by lack of nutrients in fasting or by antibiotic treatment, penetrate and damage the intestinal villi.
As it's known and proven for hyphae, i.e. the protruding fungal forms of yeasts.I had read Dr. Jennifer Daniels' short book on turpentine before.
And a couple of years ago I had already taken turpentine at 2 teaspoons per day for over two weeks. Which was a lot. I found 1 teaspoon already quite aggressive on the GI system. But I liked the "brain effects" of improved microcirculation (some headaches, though, too).I'll continue the monoterpenes in the small amounts of 4 drops multiple times daily. Doing the maths, that comes to about 1.5 teaspoons a week in total which surprisingly matches the total of Dr. Jen Daniels dosing recommendation of a 3/4 teaspoon once or twice a week.
-
@CrumblingCookie said in Oxalobacter formigens after guts nuked by antibiotics. Sources? Possibilities?:
Have you noticed anything of that?
Did you include or forego the also-mentioned L.gasseri and Bacillus subtilis?I have not noticed any dramatic changes. There is a separate thread on this forum that may be interest. L. Reuteri
I ferment L. reuteri and L. gasseri in separate batches. As a general rule, I eat a variety of fermented products 3X daily. Dr. Davis recommends 40 days to reestablish the probiotic in the gut. Thereafter, missing a day or 2 is of little consequence.
-
@DavidPS
I've ordered the BioGaia Gastrus tablets with the two L. reuteri strains to try it out.
It stands and falls with the lactose and dairy protein tolerability of the fermentation product. -
@CrumblingCookie - That is interesting. Let us know how it goes.
I think that the prolonged fermentation time would greatly reduce (but maybe not eliminate) the lactose. So it might not be as much of a issue. As for the dairy proteins, if they are a problem then consider starting with small portion. Then slowly increase the amount you eat to give your body a chance to adjust.
-
Whilst the L. reuteri are oddly fermenting (I'm not quite sure, it smells and tastes somewhat like tangy cheese), I've found a connection between GABA and the microbiome.
Essentially, not only does the notorious gut-brain-axis rely much on a GABA-producing microbiome raising GABA in serum and brain!
But a lot of bacteria of a (healthy?) microbiome exclusively depend on GABA as a crucial nutrient.
Many bacteria don't grow at all without exogenous GABA, which should be supplied by other bacteria of the microbiome.Hence, supplementing GABA feeds such bacteria and reconstitutes gastrointestinal microbiotic diversity.
And feeding GABA increases IFN-y for innate immunity, TNF-a, MUC2 for the crucial mucin barrier.
Also, feeding GABA appears to enhance autophagy of enteric cells instead of them taking the route of destructive apoptosis.GABA-producing gut bacteria are foremost Bacteroides (e.g. fragilis), Parabacteroides, Eschericia, L. plantarum, L. brevis, L. lactis, L. paracasei.
GABA content in fermented dairy (cheese) varies a lot depending on the microbiotic strains being traditionally used in the respective regions (huge differences e.g. just among the Italian Pecorino cheeses).
GABA-modulating bacteria of the human gut microbiota
I'm now supplementing c. 3grs GABA every day.
Have already felt the "heavy chest" and mild flushing for a couple of hours after my intake, as reported by others in the RPF.