Vitamin A quotes from Ray's favorite physiology book
-
A few quotes on Vitamin A from Ray's favorite physiology book, Textbook Of Endocrine Physiology By Constance R. Martin PhD.
The textbook is still downloadable from this thread: (https://raypeatforum.com/community/threads/textbook-of-endocrine-physiology-by-constance-r-martin-phd.21092/post-552642)"Cells of the thyroid gland make similar molecules.
and thyroid hormone deficiencies increase the dietary requirements for vitamin A.""Vitamin A derivatives are essential for promoting normal growth and differentiation of the epithelial cell of skin mucous membranes, reproductive organs and some sensory structures; and they exert influences on mucus secretion, keratinization, and other processes**. They deter the development of hyperplasia, dysplasia, and metaplasia and have therefore been tested for use in patients with some forms of cancer (8).** They play roles in directing growth
and remodeling of bone (82) and they protect against overgrowth at sites of innervation. Deficiencies impair skeletal development, but they are also associated with periosteal proliferation in some regions, with excessive osteoblacstic activity, and with neurological disturbances related to bone impingement on the nerves (30). Such effects are accompanied by changes in the RNA and DNA content of the tissues, and they probably involve interactions with other regulators. ""Laboratory mammals maintained on Vitamin A deficient diets stop growing, acquire numerous epithelial cell and connective tissue disorders and become blind and sterile. Retinoic acid can prevent or alleviate most of the effects, including the keratinization of the conjunctiva and failure to establish and maintain estrous cycles. However retinol or a precursor is needed for spermatogenesis, for the ability to sustain pregnancy, and for the formation of visual pigments."
-
@Mauritio Charlie would counteract with some religious hum bug about vitamin A toxicity. I really think that he does not understand physiology, yet science alone

-
@tubert He would say this is "evil whichcraft" or "more Rockefeller science"
-
Thank you @Mauritio
I'm really surprised at that first quote because I was under the impression that hypothyroidism decreases the vitamin A requirement. Do you have the page number for that quote please.
I came across this article recently - vitamin A deficiency is no small thing
Vitamin A deficiency in chronic cholestatic liver disease: Is vitamin A therapy beneficial?
-
Interesting. I suspect that vitamin a is required for the growth of any new cell, as cells that replicate the quickest seem to be most affected by deficiency.
-
It takes years to deplete VA from your body. Virtually no one on the modern world is deficient or will come even close to ever being deficient.
-
@GreekDemiGod
I don’t know why you guys say this, when the liver biopsy studies you send trying to prove that everyone has “hypervitaminosis a” generally show around 20% of the population is vitamin a deficient.https://www.sciencedirect.com/science/article/pii/S0002916522030210
“ Cadaver liver samples were analyzed to explore VA status biomarker associations in US adults. Subjects showed a high prevalence of VAD (22%) and hypervitaminosis A (33%). The WHO often uses a 20% prevalence to define a severe public health concern (33)”
https://pubmed.ncbi.nlm.nih.gov/3219311/
“Of all the samples 16% contained less than 40 mg/kg, 45% had 100-300 mg/kg, while 9% contained more than 500 mg/kg liver.”
I can cite other studies, but most countries find similar results.
-
@jamsey is this micro grams? (ug)
-
@Mauritio Thank you for sharing the Constance Martin book link.
-
@Jakeandpace
Milligrams. These are liver biopsy numbers -
@Peatly Interesting study although I’m not sure if it agrees with the Low A crowd or disagrees. I don’t know enough to comment but it seems it could fit into their paradigm
“Nevertheless, the only study describing hepatic vitamin A levels in PBC patients showed that retinoids accumulate in HSCs.24Nyberg et al.24 confirmed that PBC patients have lower serum retinoid levels than controls and that these levels correlate with the stage of disease. Additionally, they found that HSCs are larger and more numerous in PBC patients in comparison with the controls. Also, while serum retinol binding protein (s-RBP) staining intensity was comparable to control intensity, staining intensity of cellular RBP (c-RBP) was significantly enhanced in PBC patients. This suggests that the release of retinoids from HSCs may be restrained in PBC. The lack of stimulatory effects of estradiol on the hepatic secretion of RBP during menopause may further explain why PBC affects primarily elderly women.5, 25 In 2000, Erickson et al.26 suggested that vitamin A toxicity may contribute to the aetiopathology of PBC. Intrahepatic cholestasis caused by vitamin A intoxication has been reported in two cases,27, 28 and interestingly, in one case hypervitaminosis A was cured by the application of UDCA.28”
-
@GreekDemiGod gay
-
@Jakeandpace Thank you for reading. The study concludes:
Vitamin A metabolism and cholestatic disorders are connected in a certain way, since vitamin A deficiency in chronic cholestatic diseases may be not only a reflection of reduced gastrointestinal absorption of fat-soluble vitamins, but it also could be involved in the pathological mechanisms underlying these diseases. In cholangiopathies, retinoids exert their potentially beneficial effect through different mechanisms: repression and prevention of hepatic fibrosis after liver injury through the inhibition of Ito cell transformation into myofibroblasts, modulation of the immunological response to hepatic damage through the regulation of expansion and apoptosis of myeloid cells, and the reduction of the toxicity of cholestasis through the inhibition of bile salt synthesis. More research is needed on hepatic retinoid levels of patients with chronic cholestatic diseases. Also, different retinoids and application forms may exert different effects and have yet to be investigated, including potential severe adverse effects. However, atRA may be a promising new agent in the therapy of chronic cholestatic disorders.atRA (all-trans retinoic acid)
-
@Peatly Yes good point . You would expect the opposite. Not sure why that would be. Can Vitamin A substitute for thyroid hormone ?
-
@Mauritio Well, I'm not sure. It does seem to modulate the thyroid but not in the way I had previously understood it. I’m yet to understand the full mechanism by which thyroid deficiency may warrant more vitamin A but I am reading and hope to report back.
The relationship between thyroid disorders and vitamin A.: A narrative minireview
From the article
“Retinoid nutritional status is able to modulate thyroid gland homeostasis. Vitamin A deficiency (VAD) appears to be closely related to thyroid gland impairment, due also to its frequent association with iodine deficiency (ID) (3, 4, 6, 10). Indeed, retinoids seem to play a role in the development and maturation of the thyroid cell phenotype (4).”
“Several animal studies using mouse models have shown that VAD is related to reduced iodine uptake, impaired coupling of iodothyronines, and reduced thyroglobulin synthesis, which can lead to thyroid hypertrophy and goiter and to a decreased intrathyroidal pool of T3 and T4 (10–15). The hypothesis that vitamin A deficiency, in the presence of protein-calorie malnutrition, might impair the glycosylation of thyroglobulin (Tg) was proposed by Ingenbleek Y in 1983 (12).”
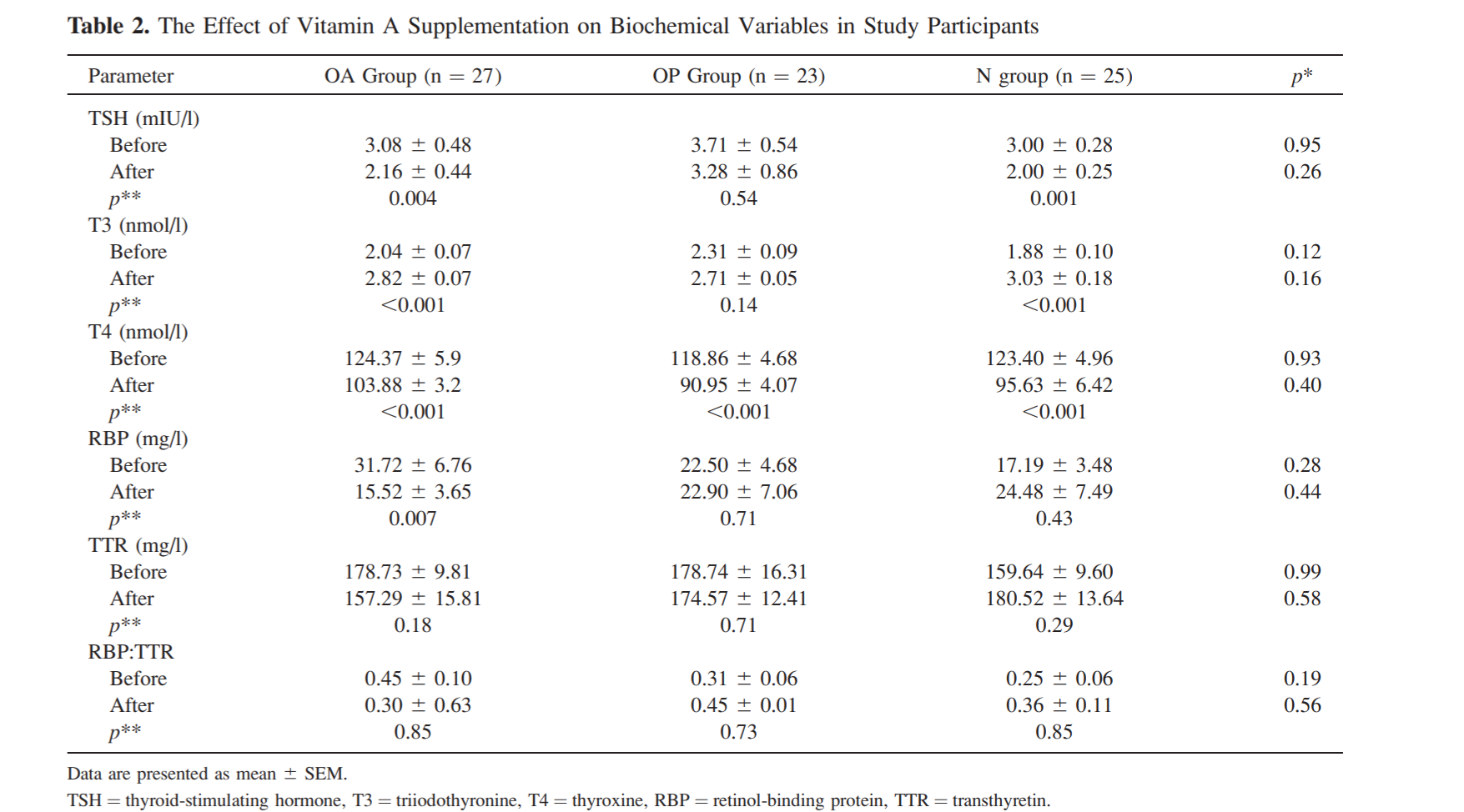
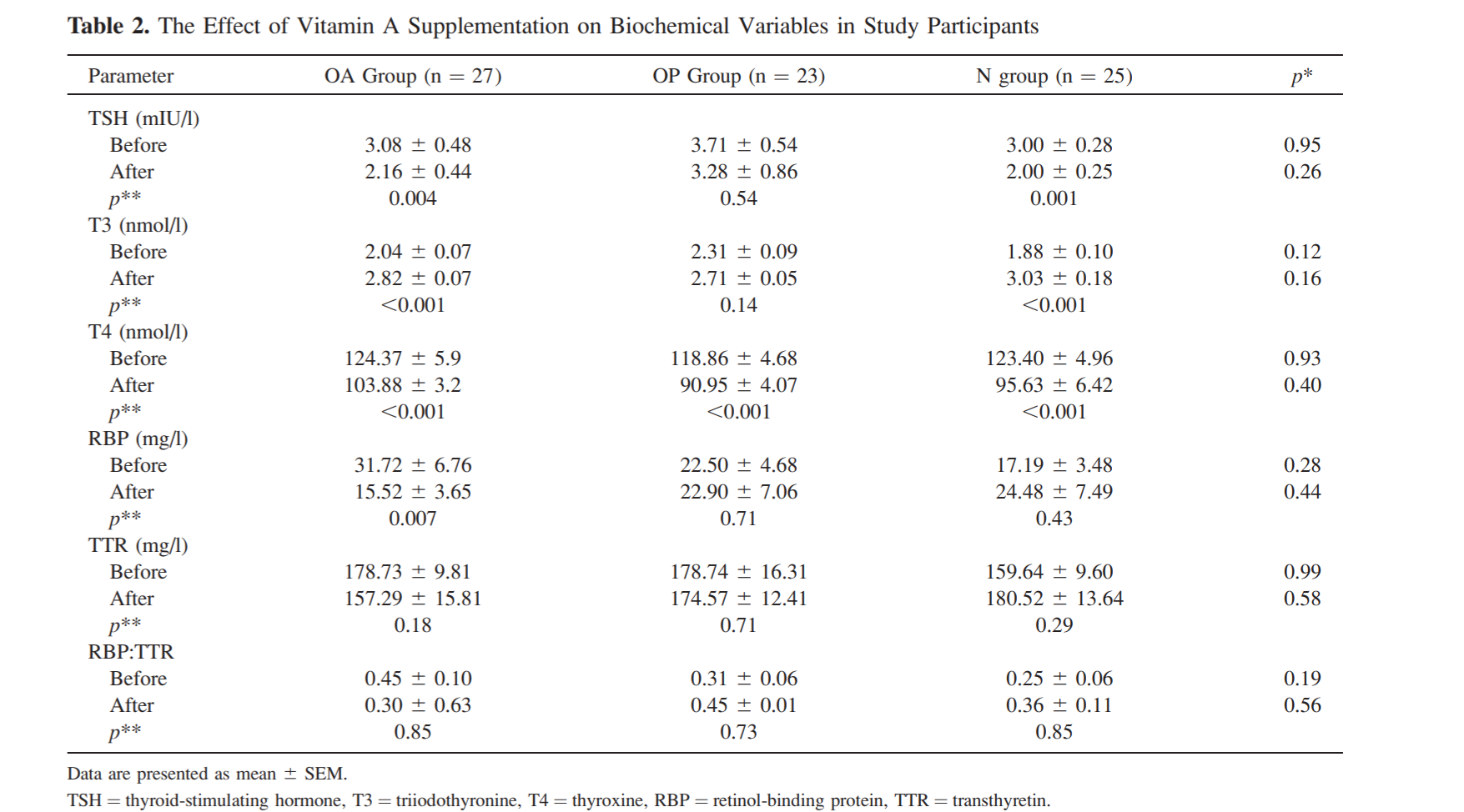
“A relatively recent Iranian study by Farhangi et al. observed that, in healthy premenopausal obese and non-obese women, 4 months of VAS was able to reduce TSH and increase T3 levels (possibly due to a hepatic effect on the conversion of thyroid hormones), reducing the risk of subclinical thyroid dysfunction (32).”
For some reason I can't find that first quote in the Constance R. Martin book
-
@Peatly Wow , very interesting!
Especially those two quotes:@Peatly said in Vitamin A quotes from Ray's favorite physiology book:
“Several animal studies using mouse models have shown that VAD is related to reduced iodine uptake, impaired coupling of iodothyronines, and reduced thyroglobulin synthesis, which can lead to thyroid hypertrophy and goiter and to a decreased intrathyroidal pool of T3 and T4 (10–15).
@Peatly said in Vitamin A quotes from Ray's favorite physiology book:
“A relatively recent Iranian study by Farhangi et al. observed that, in healthy premenopausal obese and non-obese women, 4 months of VAS was able to reduce TSH and increase T3 levels
-
This study shows that high doses of Vitamin A do lead to hypothyroidism (lowered T3, T4, increased TSH) in a dose-dependant manner.
Now the authors were aware of the pro-thyroid effects Vitamin A has in lower doses, so they wanted to see what higher doses did.
The HED I calculated for the lowest dose was about 30 000 IU per day, so not extremely high, yet it still clearly had a visible anti thyroid effect.
I would have liked to see one with 5 or 10 000 IU, which is a much more realistic dose."It has been known that vitamin A deficiency affects thyroid hormones for many years, resulting in iodine deficiency disorders, while vitamin A supplementation alleviates the risk of subclinical hypothyroidism [23, 24]. Recently, a study has been conducted to investigate the relationship between vitamin A and thyroid function in obese individuals. Vitamin A deficiency is more common in subjects with obesity and is significantly related to thyroid dysfunction. Adequate vitamin A levels improved thyroid function in obese subjects with subclinical hypothyroidism [25]. However, no study has focused on the association between vitamin A overload, thyroid dysfunction, and insulin resistance. Therefore, the current study aimed to investigate the effect of prolonged and high doses of vitamin A on thyroid function and glucose metabolism.
-
@Mauritio said in Vitamin A quotes from Ray's favorite physiology book:
“A relatively recent Iranian study by Farhangi et al. observed that, in healthy premenopausal obese and non-obese women, 4 months of VAS was able to reduce TSH and increase T3 levels
@Peatful this is the study that you referenced above, which shows a beneficial effect of 25 000 IU of Retinyl palmitate on thyroid markers, meaning increased T3 and lowered TSH.
Its interesting that the rat study found negative effects and the human study postive effects at a similar dosage.
But since human studies are higher up in the evidence pyramide, I tend to interpret this as Vitamin A beeing good for thyroid in reasonable dosages.The effect was especially pronounced in nonobese individuals where T3 increased by more than 60%!
-
"In the vitamin A-deficient rats, the thyroid weight increased and the level of serum thyroxine decreased to one half that of the control rats. Normal thyroid weight and serum thyroxine levels were recovered by the replenishment of retinyl palmitate in the vitamin A-deficient rats. In addition, decreased hormone synthesis was observed in the thyroid glands of the vitamin A-deficient rats."
-
@Mauritio said in Vitamin A quotes from Ray's favorite physiology book:
@Mauritio said in Vitamin A quotes from Ray's favorite physiology book:
“A relatively recent Iranian study by Farhangi et al. observed that, in healthy premenopausal obese and non-obese women, 4 months of VAS was able to reduce TSH and increase T3 levels
@Peatful this is the study that you referenced above, which shows a beneficial effect of 25 000 IU of Retinyl palmitate on thyroid markers, meaning increased T3 and lowered TSH.
Its interesting that the rat study found negative effects and the human study postive effects at a similar dosage.
But since human studies are higher up in the evidence pyramide, I tend to interpret this as Vitamin A beeing good for thyroid in reasonable dosages.The effect was especially pronounced in nonobese individuals where T3 increased by more than 60%!