Random, interesting studies
-
HPβCD = 2-Hydroxypropyl-beta-Cyclodextrin = OHp-betadex has some interesting properties.
As the other cyclodextrins it provides hydrophilicity outside but the ability for hydrophobic compounds to lodge in its inner core. While the OH-p extension AFAIK widely prevents its deconstruction to glucose by amylases and makes for higher solubility in water compared to simple cyclodextrins.
The cyclodextrins seem to provide an especially outstanding fit for binding lipids (fatty acids).
Plus they have been shown to stimulate autophagic flux. Maybe both mechanisms work hand-in-hand.Here's a self-experimenter's case report of 18 i.v. treatments over 36 days as a 20% in 0.9% NaCl solution:
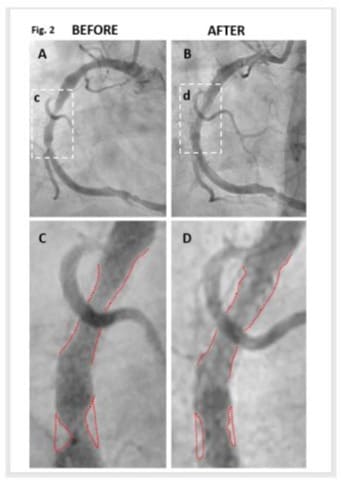
2-Hydroxypropyl-Β-Cyclodextrin Reduces Atherosclerotic Plaques in Human Coronary Artery
It also appeared to improve renal functions wrt albumin retention.There's a MD James C. Roberts who has collected a few more bits on such atherosclerosis reversion on his website: https://www.heartfixer.com/IndexCHC.htm
-
@CrumblingCookie Thanks; this is useful information. Heartfixer.com had dropped off my radar screen.
-
A pulsed magnetic field was more effective for biliary sludge (gallstone precursor) then medicamentous therapy.
-
-
@Mauritio for some reason it makes my foot hurt in a plantar facitis manner
-
@lobotomize-me what ?
-
@Mauritio eating pomegranates makes my foot ache
-
Pharmacological correction of obesity-induced autophagy arrest using calcium channel blockers
https://pmc.ncbi.nlm.nih.gov/articles/PMC4157315/
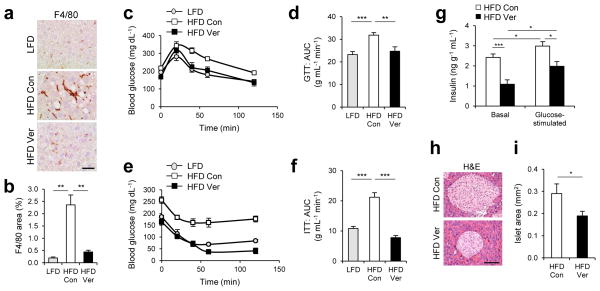
4 month-old C57BL/6 male mice kept on HFD for two months were subjected to daily administration of PBS (Con, n = 4) or verapamil (Ver, 25 mg kg−1 body weight, i.p., n = 3) for 10 days. LFD-kept mice of same age (n = 5) were used as a negative control. (a, b) Liver sections were subjected to F4/80 immunostaining, which visualizes macrophage infiltration and hematoxylin counterstaining (a). F4/80-positive areas were quantified (b). (c–f) Glucose tolerance tests (GTT, c, d) and insulin tolerance tests (ITT, e, f) were conducted using indicated mice (c, e). Area-under-the-curve (AUC) was quantified from GTT and ITT data (d, f). (g) Serum insulin levels were measured from indicated mice before (Basal) and 10 min after (Glucose-stimulated) glucose injection (n = 4). (h, i) Pancreas sections were analyzed by hematoxylin and eosin (H&E) staining (h). Islet areas were quantified (i) (n = 4). Scale bar, 200 μm (a), 100 μm (h). All data are shown as mean ± s.e.m. *P < 0.05, **P < 0.01, ***P < 0.001 (Student’s t test).
[The high fat diet effects were brought about by palmitic acid. PUFA-involvement not required.]
However, we should take into account that, even though autophagy is important for prevention of metabolic pathologies and diabetes, autophagic defects, which are correctable by calcium channel blockers, may not be the only cause for diabetes. Thus, it is feasible that calcium channel blocker-mediated restoration of the autophagic flux could not prevent the occurrence of incidental diabetes in certain cases as they may have arisen from causes other than autophagy misregulation. Nevertheless, our study does suggest that calcium channel blockers have a clinical potential for a subset of patients with NASH and type 2 diabetes whose symptoms are indeed associated with lipotoxicity-induced autophagy arrest.
-
@CrumblingCookie No, the effects were not induced by palmitic acid. You misread that, as the palmitic acid is typically used as a reagent just like in this study. This is more so a case of sleight of hand with the common, "let's see how such and such thing affects metabolism or health, while we feed them high PUFA in the background." The mice had access to the common 'chow' bullshit they use in these studies. Chow is predominantly unsaturated fat. In the case of the HFD, these mice had exposure predominant amounts of C18:2 aka Linoleic acid. The so-called LFD is also mostly comprised of soybean oil.
Calcium efflux is one known mechanism of stress, which is calcium going to the wrong places; calcification. In a very specific way, when protein folding is disturbed for example, it can trigger this process. PUFA is notorious for disturbing protein synthesis as well as proper folding. This study showed, pufa exposure leading to this detrimental effect, being mitigated by calcium channel blockers. It's not news or a surprise. But better things like magnesium and or the reduction of pufa intake are better strategies,
-
@bio3nergetic
I welcome your scepticism on this as I have myself seen the various and notoriously misleading studies wherein predominantly polyunsaturated FAs were foisted on the readers as a diet of saturated FAs.
With regard to autophagy however there's a distinctly inhibiting role of palmitic acid especially, it seems, according to the paragraph below and the supplementary data of the in-vitro part of this study (and others). Oleic acid or DHA did not have the same effect. They did not analyse linoleic acid's isolated effect in this and we can assume that LA is the worst but this doesn't take away the findings that PA brings about the described effects on its own. Perhaps the in-vivo results about systemic glucose and insulin will be less extreme with a different HFD richer in PA but PA's still particularly inhibitive. I agree there could be an inconsequentuality between the in-vitro reasoning and the in-vivo feeding,
yet I've looked up the chow they've used in this study for the HFD: S3282, Bio-Serv :Lard, Casein, Maltodextrin, Sucrose, Mineral Mix, Vitamin Mix, DL-Methionine, Choline Chloride
It's lard-based, which to my knowledge typically only has about 12% PUFA, and you'd probably call this ingredient list "peaty", wouldn't you? Well except for the methionine amino acid balancing.
The authors state that the mechanism here is due to inhibition of SERCA by decreasing ER membrane fluidity due to PA. Alleviating ER-stress in particular by various compounds did not negate the inhibition. It was specifically due to SERCA."During obesity and NASH, excessive fat accumulation inside hepatocytes can provoke formation of protein inclusions consisting of p62 and ubiquitinated proteins24, 28. Since the process of inclusion body formation was yet to be explored, we devised an in vitro system that made it possible to examine the effect of lipids on protein aggregation. We found that, in response to palmitic acid (PA, 500 μM), which is a long-chain saturated fatty acid (SFA) that becomes highly elevated in sera of obese individuals, human HepG2 hepatoma cells formed a considerable amount of insoluble cytoplasmic inclusions consisting of ubiquitinated proteins and p62 (Fig. 1a–c). PA-induced accumulation of protein inclusions had a proportional correlation with both dose (Supplementary Fig. 1) and time (Supplementary Fig. 2a); correspondingly, when treated for a longer period (48 hr), even a very low dose of PA (50 μM) was able to induce substantial protein inclusions (Supplementary Fig. 1b). Although prolonged treatment of high-dose PA (24 and 48 hr, 500 μM) provoked apoptosis, there was no significant cell death at 9 hr of PA treatment (Supplementary Fig. 3), a time point at which we observed the greatest amount of prominent protein inclusions (Fig. 1a–c and Supplementary Fig. 2a). The inclusions were frequently associated with condensed fibers of keratin (Supplementary Fig. 4a) or tubulin (Supplementary Fig. 4b) as observed previously for various protein aggregates28, 30. It is interesting to note that the protein aggregates were located away from the endoplasmic reticulum (ER) structure (Supplementary Fig. 4c) in which many unfolded proteins typically accumulate during lipotoxicity and obesity13. Although another SFA stearic acid (SA) was also able to induce accumulation of p62 (Supplementary Fig. 2b), unsaturated fatty acids (UFA) such as oleic acid (OA) and docosahexaenoic acid (DHA) failed to induce such accumulation (Supplementary Fig. 2c, d) and actually suppressed the effect of SFA (Supplementary Fig. 2e, f)."
"SFA, but not UFA, induced prominent accumulation of autophagosomes as manifested by increased LC3-II levels (Supplementary Fig. 2a–f). "
Do you think we should all focus more on not to neglect MUFA/oleic acid therefore rather than praising and binging on SFA?
-
@CrumblingCookie I think that we shouldn't let the main plot get away from us as we get lost in the weeds. There are numerous things that new-fangled research gets us in the weeds about by starting with a premise involved in minutia and creating alarms based on observed effects. While this can have value as side or mental notes in research, we shouldn't forget the big picture. The problems these types of studies create are one of non-real conditions. In fact, the overwhelming conclusion we ought to draw from all studies on PA should indicate to use autophagy inhibition by PA occurs under lipotoxic conditions i.e. HFD exposure. It is within the context of lipotoxicity due to fats that they are trying to prove the toxicity of yet another fat: in isolation; at very high doses, not normal food consumption. In contrast actual dietary fats, as in food, contain a mix of fatty acids and are metabolized differently, often mitigating such effects and presenting with opposite effects. Just look at the liver protective effect studies of PA.
At best, even in studies where it is not high, unreal, isolated doses what they establish are markers of preconceived notions to then derive their conclusions. This is classically begging the question. For example the 2019 randomized crossover trial in The American Journal of Clinical Nutrition tested diets with ~30% fat energy, where ~50% of that fat came from PA, stearic acid, or OA all within feasible dietary ranges. It found PA raised LDL and non-HDL cholesterol compared to OA and stearic acid. "Cholesterol especially bad cholesterol (as they cringely say) is bad, therefore PA is bad." Meanwhile, the bigger picture stuff confesses: no difference in inflammation or immune markers.
Recall, even Peat spoke out against the fad of autophagy as a craze. Because in the pro metabolic view or bioenergetic view, phagocytic activity which is the host of immune components, is much more vital. And those components are built up by good diet and nutrients. Autophagy should be seen as a last resort of sorts, ideally very background process, that - not as an intentionally overt, self-induced process - is regulated by said bioenergetic system. Chronic fasting for example would be one such way in inducing stress to overtly induce autophagy. The real questions should be about total effects on the thriving of an organism. I think speaking of obesity as a [proven] hinderance to a specific organism is more valuable than questioning whether or not a certain degree of autophagy has taken place.
-
@bio3nergetic
I appreciate your reply on this. It's interesting.Recall, even Peat spoke out against the fad of autophagy as a craze. Because in the pro metabolic view or bioenergetic view, phagocytic activity which is the host of immune components, is much more vital. And those components are built up by good diet and nutrients. Autophagy should be seen as a last resort of sorts, ideally very background process, that - not as an intentionally overt, self-induced process - is regulated by said bioenergetic system.
And I hold RP as a fool for such belittlement and neglect. It's of no help to focus on healthy-people talk and how things ought to be with denial of chronic disease states from other reasons. E.g. what was his take on tuberculosis?
There's no effective phagocytic activity without functioning (xeno)autophagy following up the phagocytic internalisation. Yes, ideally it should be a continous background process which clearance just as necessary, without a harmful build-up which then causes harm and further inhibition by its own mechanisms other than those which led to such a clogged system.Please correct me if I'm wrong in reading much of what your saying as a call to not get hold up with specific mechanisms to override the importance of the wider (dogmatic) achievements.
It's important to not fall for discussing the forest as an abstracted whole whilst denying the very substantial need of individual trees. -
@CrumblingCookie I think you're oscillating unnecessarily between two extremes, running the meaning and purpose of a given background system and applying it disproportionally to proactive health choice. Peat's sentiment about autophagy isn't "neglect" or "belittlement," nor is he saying it isn't important, but rather the emphasis on not intentionally pushing certain systems out of context because stress brings about an induction of said system with the loaded premise that, that system being pushed is good. Autophagy - and in context of effective phagocytic activity - takes care of itself with an over-arching nutritional/bioenergetic application. When you get that right, those systems purr right along as they should. When you prolong fast; "artificially fast as I put it chronically, you are pushing those systems out of context. This will not give you good results. In these out-of-contexts scenarios, the cell is eating its own apparatus, regardless of its state because the stress signal and uncoping of that stress dictates that. What you describe is preaching to the choir. What should be emphasized is good health/bioenergy to ensure those systems do their thing WITHIN context, in which, things you describe apply and for the good of the organism. It is always about the whole forest. You can get lost in the trees themselves or worse - as I suspect with a lot of these worthless studies - you can easily create an "allegory of the cave" type situation: they beguile you with shadows and red herrings. What fascinates me is how easy it is in life to do so.
-
Lanolin/cholesterol rich diet protects from osteonecrosis.
https://pubmed.ncbi.nlm.nih.gov/24171681/ -
@Mauritio,
Vitamin E prevents steroid-induced osteonecrosis in rabbits
Found in the 'Similar articles' in pubmed.
The experiments seem to corroborate the ones in the 'CHOL article':
In the Control group 15 out of 30 had the osteonecrosis, while in the alpha-tocopherol one 5/20.I suppose the Vitamin E + high-cholesterol (lanolin) would be the best diet.
-
Topical Oxidized Vitamin C (DHA) permeates through skin 12x faster than ascorbic acid.
Even though the human study below is from a company that produced the product with DHA, it seems to be very carefully done with practical considerations.
-
@Lejeboca yes I saw that one too but hadn't clicked on it. Thanks for sharing.
-
Sorbitol
I'd be careful with sorbitol. The issue with sorbitol is that it is often made with a nickel catalyst, which leaches into the endproduct.
" The Cr/Fe promoted system exhibits the highest activity but the Fe leaches from the catalyst into the reaction mixture. Moreover, this catalyst deactivates after successive runs. For all Raney-type Ni catalysts leaching of Ni in the product mixture occurs."
https://www.sciencedirect.com/science/article/abs/pii/S0920586103000403?via%3DihubAlthough Ray said a little is ok:
Post 28 Title: Bryan · Feb 4, 2013 at 5:00 PM Author: Bryan Post Content:
Me: Is sorbitol o.k. to eat? I got some gummy bears that have it in them.
Peat: A little is o.k.
-
Papaya/Papain
Papain reverses the effects of a high fat diet in mice. The mice getting Papain, did not gain more weight than the mice on a normal control diet.
Papain even lowered visceral fat content slightly below the control group.
It lowered liver enzymes, triglycerides, adipogenic and inflammatory Markers.
It also drastically upregulated AMPK, similarly to aspirin, biotin or infrared light.https://pmc.ncbi.nlm.nih.gov/articles/PMC8468764/
Potent Fibrinolytic, Anticoagulant, and Antithrombotic Effects of Papain
https://pubmed.ncbi.nlm.nih.gov/38069092/Lowers the number of mast cells and inflammatory cytokines
https://pubmed.ncbi.nlm.nih.gov/39199175/Papain has anti-artherosclerotic effect. Lowers COX-2, PGE2 and other cytokines.
https://pubmed.ncbi.nlm.nih.gov/36947095/Papaya extract increases testosterone and sperm health, damaged by alcohol.
https://pmc.ncbi.nlm.nih.gov/articles/PMC7099107/#Sec17Papain had anti fungal effects against different fungi, including ringworm.
https://pmc.ncbi.nlm.nih.gov/articles/PMC3209867/
https://pmc.ncbi.nlm.nih.gov/articles/PMC11128596/Papaya extract has anxiolytic effect
Evaluation of anxiolytic and sedative effects of 80% ethanolic Carica
papaya L. (Caricaceae) pulp extract in micePapaya extract has anti-depressant effect and lowers body weight.
https://pubmed.ncbi.nlm.nih.gov/40457195/
Papaya extract has anti depressnt effect. Lowers lipid peroxidation, increases catalase.
https://ijprajournal.com/issue_dcp/Screening of Antidepressant Activity of Ethanolic Extract of Carica papaya L. Leaves in Rats.pdfPapaya extract ameliorates a lot of the conditions bright on by sodium flouride on the brain and neurorransmitters.
https://phcog.com/article/sites/default/files/PhcogMag1455123-2802918_074709.pdf -
Oyster peptides increase testosterone
https://pmc.ncbi.nlm.nih.gov/articles/PMC10563733/