@yerrag said in Thymus health:
was it to calm the cytokine storm as a way to dampen Inflammation? I just know cortisone is used as an anti-inflammatory but don't know the mechanism.
Below is a study that considers the dual pro- and anti-inflammatory effects of cortisol under stress with respect to the time of introduction of immune challenge (LPS), It also notes the mechanism of upregulating TLRs, which recognize pathogen molecular patterns, in the brain and liver.
Prior exposure to glucocorticoids sensitizes the neuroinflammatory and peripheral inflammatory responses to E. coli lipopolysaccharide
Abstract
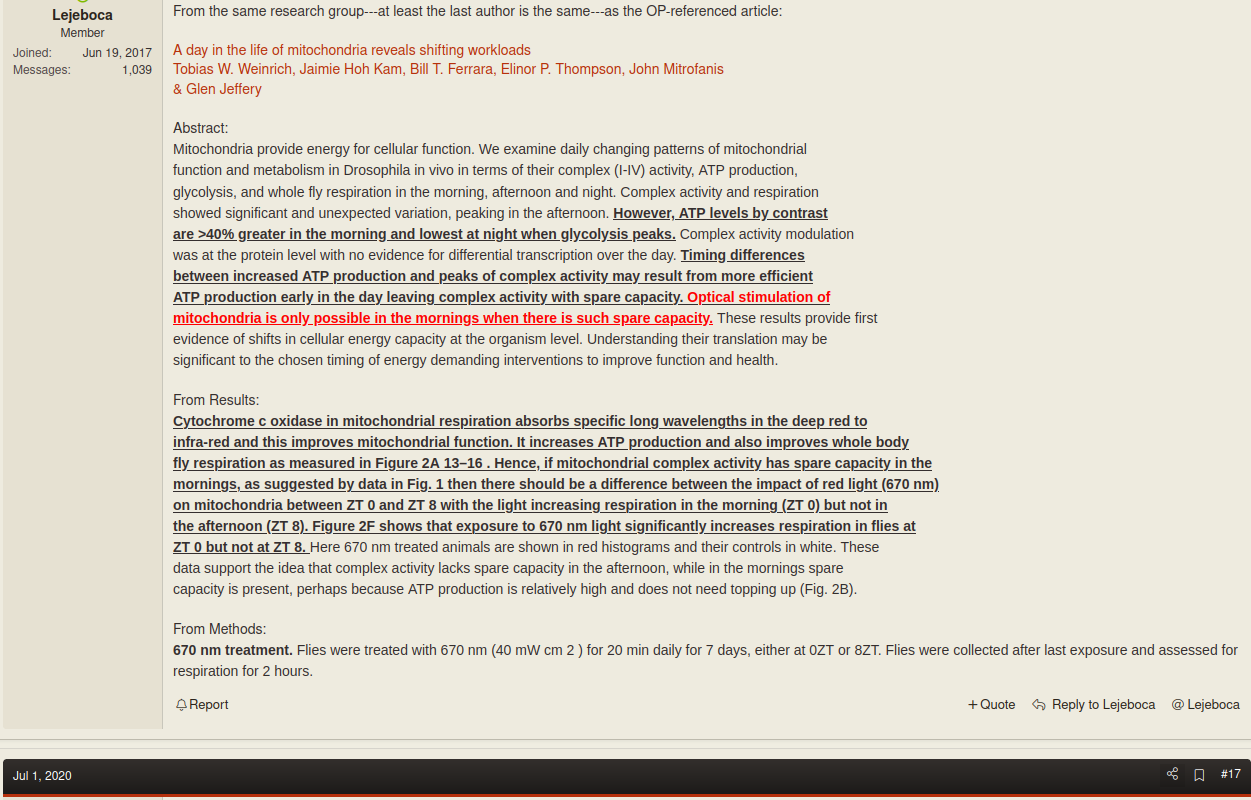
Acute and chronic stress has been found to sensitize or prime the neuroinflammatory response to both peripheral and central immunologic challenges. Several studies suggest that stress-induced sensitization of neuroinflammatory processes may be mediated by the glucocorticoid (GC) response to stress. GCs, under some conditions, exhibit pro-inflammatory properties, however whether GCs are sufficient to prime neuroinflammatory responses has not been systematically investigated. In the present investigation, we tested whether acute administration of exogenous GCs would be sufficient to reproduce the stress-induced sensitization of neuroinflammatory responses under a number of different timing relationships between GC administration and immune challenge (lipopolysaccharide; LPS). We demonstrate here that GCs potentiate both the peripheral (liver) and central (hippocampus) pro-inflammatory response (e.g. TNFα, IL-1β, IL-6) to a peripheral immune challenge (LPS) if GCs are administered prior (2 and 24 h) to challenge. Prior exposure (24 h) to GCs also potentiated the pro-inflammatory response of hippocampal microglia to LPS ex vivo. In contrast, when GCs are administered after (1 h) a peripheral immune challenge, GCs suppress the pro-inflammatory response to LPS in both liver and hippocampus. GCs also up-regulated microglial activation markers including Toll-like Receptor 2. The present data suggest that the temporal relationship between GC treatment and immune challenge may be an important factor determining whether GCs exhibit pro- or anti-inflammatory properties.
Although the study considered a pretty high dose of cortisol (CORT), smaller (and chronic) doses would have a similar effect, in its nature, *the authors fixed the measurements at 4h of LPS introduction.
A dose of CORT was chosen that had previously been determined to mimic the plasma CORT profile produced by an acute stressor (a session of 80–100 inescapable tailshocks) (Fleshner et al., 1995). We had found that this acute stressor potentiates the neural and peripheral inflammatory responses to LPS administered 1–4 days later (Johnson et al., 2002).