Mysterious gallbladder disease - can't digest fat for no apparent reason
-
This post is deleted! -
@random Can't quench my thirst, yes. But also other symtpoms like very dry skin, dry eyes, heat intolerance, exhaustion, sometimes confusion... In the past, I was drinking up to a quart of milk a day, but lost my ability to digest milk sometime around 2021
-
@BearWithMe said in Mysterious gallbladder disease - can't digest fat for no apparent reason:
@random Can't quench my thirst, yes. But also other symtpoms like very dry skin, dry eyes, heat intolerance, exhaustion, sometimes confusion... In the past, I was drinking up to a quart of milk a day, but lost my ability to digest milk sometime around 2021
I got unquenchable thirst drinking raw milk+ sun exposure, sometimes you need more liquid, if liquid doesnt quench your thirst you need more nutrients. sometimes organs Can make the thirst disapear, and sometimes sun exposure specifically midday increase it
-
@CrumblingCookie Sometimes the food sits in my stomach for 2 days (no exaggeration). There is definitely something wrong with my peristaltis. The GI issues are also highly correlated to "stickyness" of the food I eat. I can digest rice noodles without issue (as they are very slippery), but plain rice (sticky) would sit in my stomach forever. I can digest any kind of pasta without problems (wheat, corn, rice...), but porridge made from the same grain would sit in my stomach forever.
I was tested for H. pylori and gastric/duodenal ulcers in 2014 (upper GI endoscopy). I was not tested for blood in stool, calprotectin or bacterial intestinal pathogens. No enlargement seen on the ultrasound. My liver is abnormally small.
I think bile helpers improved the floating stool.
-
@BearWithMe said in Mysterious gallbladder disease - can't digest fat for no apparent reason:
@random Can't quench my thirst, yes. But also other symtpoms like very dry skin, dry eyes, heat intolerance, exhaustion, sometimes confusion... In the past, I was drinking up to a quart of milk a day, but lost my ability to digest milk sometime around 2021
Did you already have thèse symptoms in 2021?
-
There is an hormone called secretin which is linked to peristalsis, bile and water homeostasis.
It tends to slow digestion in the stomach but with respect to water homeostasis, it's more anti-diuretic.
-
@CrumblingCookie I'm struggling to find any lab that would do the tests you mentioned (Eastern Europe), but will continue searching.
What would be the best course of action in the situation you described?
For the mucosal infection, I'd assume some kind of antibiotic / antifungal, but one have to be very careful not to make things worse? Having the bacterial intestinal pathogens test done would be useful also because one can precisely target the specific pathogen?
How can be fixed broken forward peristaltis?
-
@BearWithMe
Calprotection as an inflammatory marker should be widely available?
For the bacterial pathogens (nowadays it's usually a single multiplex-PCR kit being used) maybe look for yersinia, campylobacter, enteramoeba etc. which are covered by it. Yeasts or specifically candida-antigen in stool is separate.
H. pylori could be detected with a blood antibody at-home quick test (one of those little laminar flow kits) or per antigen in stool sent in to a laboratory. If you can't get another gastroduodoscopy.
Yes it would be helpful to narrow down what it is. Or narrow down what it isn't.
By all the antiparasitic things you have thrown at it it's more likely bacterial or fungal or malignant or chemically induced.
If there's no specific pathogen to be found maybe it's "tropical sprue" which essentially is SIBO and treated with doxycyclin or rifaximine. Those are on the more alright side of the antibiotic range. Camphoric acid or haidut's CamphoSal could be nonspecific treatment. If it's (nonspecific) anaerobes, teicoplanin or nitazoxanide could be an idea. If it's fungal, generous amounts of nystatin and/or generous amounts of borax for a while. Things would become much more extensive in case of intestinal Tb. It can't really be bile acid malabsorption as that would lead to chologenic diarrhea from bile stimulation, not constipation.
Weirdly, most infectious scenarious should lead to diarrhea, which you don't complain about and so there's something confounding going on.
GABA (powder) promotes downward(forward)-peristalsis.
Sufficient dietary choline could be necessary (acetylcholine signalling). Sufficient serum B12 is always essential. -
@CrumblingCookie That was super informative post. Thank you. Appreciate your comments very much! Will try to get the pathogen diagnosed and treated according to your recommendations.
I have textbook symptoms of decreased GABA activity, minus epilepsy and seizures. I had these symptoms since I was born, long before my digestive issues started. My digestive flareups seems to coincide with restlessness, insomnia, depression, anxiety and autism flareups.
Is taking GABA powder enough to fix this? Should I take vitamin B6 + magnesium + maybe Bifidobacterium adolescentis-containing probiotic?
-
@BearWithMe
No problem. Lots of bacteria of the microbiome can synthesize GABA and I think of the B. adolescentis as one of the overall better ones but imo it's no good or at the least no benefit to feed colon-colonizing bacteria whilst there's something wrong in the upper GI system. P5P can be nice but I'd want to affirm serum B12 to be >500 ng/L first (wrt peristalsis).
Out of curiosity: Which antiparasitics had you taken? Any pancreatic lipotomatosis seen in the ultrasound? Afaik pancreatic secretion and gastric acid secretion are correlated so anything disrupting one of them would inhibit the other (wrt to the gastroparesis or lack of gastric mucous layer (impact of food stickyness) you wrote).I hope you can figure things out and share your findings.
-
@CrumblingCookie Makes sense. Also, the antibiotics I might have to take would probably eradicate any B. adolescentis succesfully planted in the digestive tract.
Regarding antiparasitics, I have taken only flowers of sulphur, but in quite high doses (approx. 2x-3x the recommended antiparasitic dose) and the courses were repeated to increase chances of hitting the parasites in the right moment of their life cycle. Should I try different antiparasitic?
To summarize the discussion so far: I should take GABA powder and ensure adequate b12 + choline, to support forward peristaltis. Figure out what kind of pathogen colonized my digestive tract (if any) and then use targeted therapy to eradicate that pathogen, and/or use Camphoric acid as a non-specific treatment. Is that correct?
GABA powder cures my insomnia within minutes of taking, btw.
Would you recommend taking monolaurin as an adjuvant therapy, to support the main antibiotic / antifungal?
Earlier you mentioned chemically induced GI issues, what kind of chemicals might induce such symptoms?
I was told that there was no pancreatic lipotomatosis seen in the ultrasound.
Pancreas:

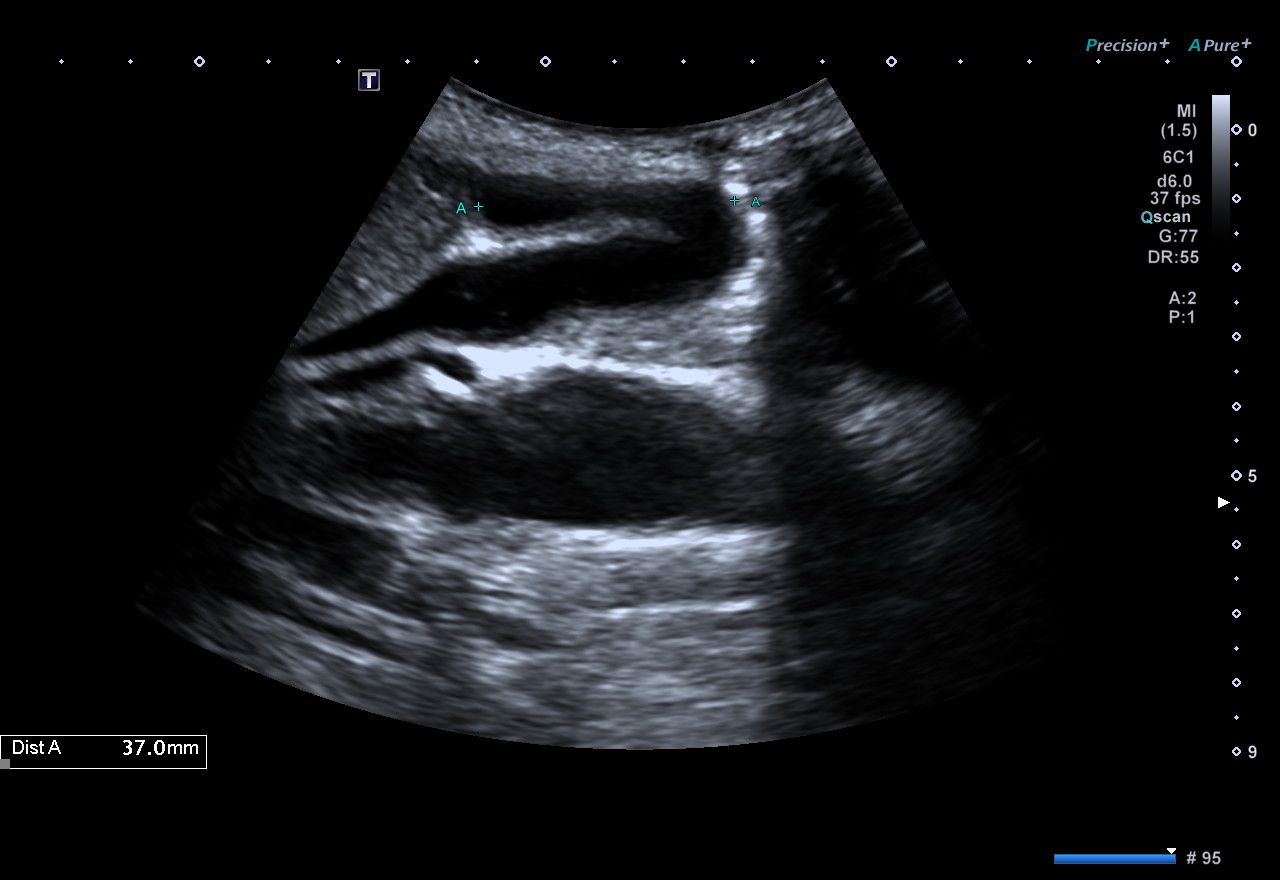
Gallbladder:
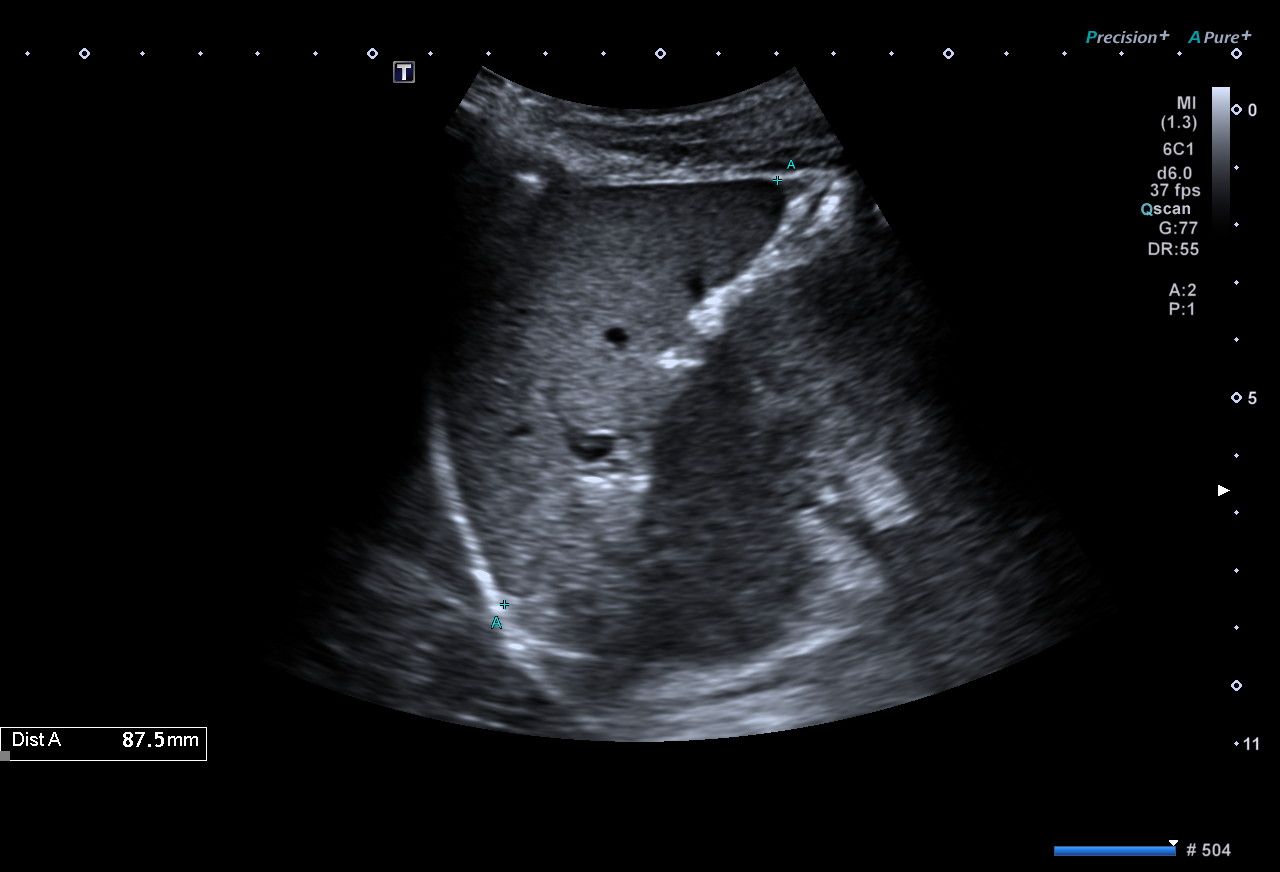
Liver:
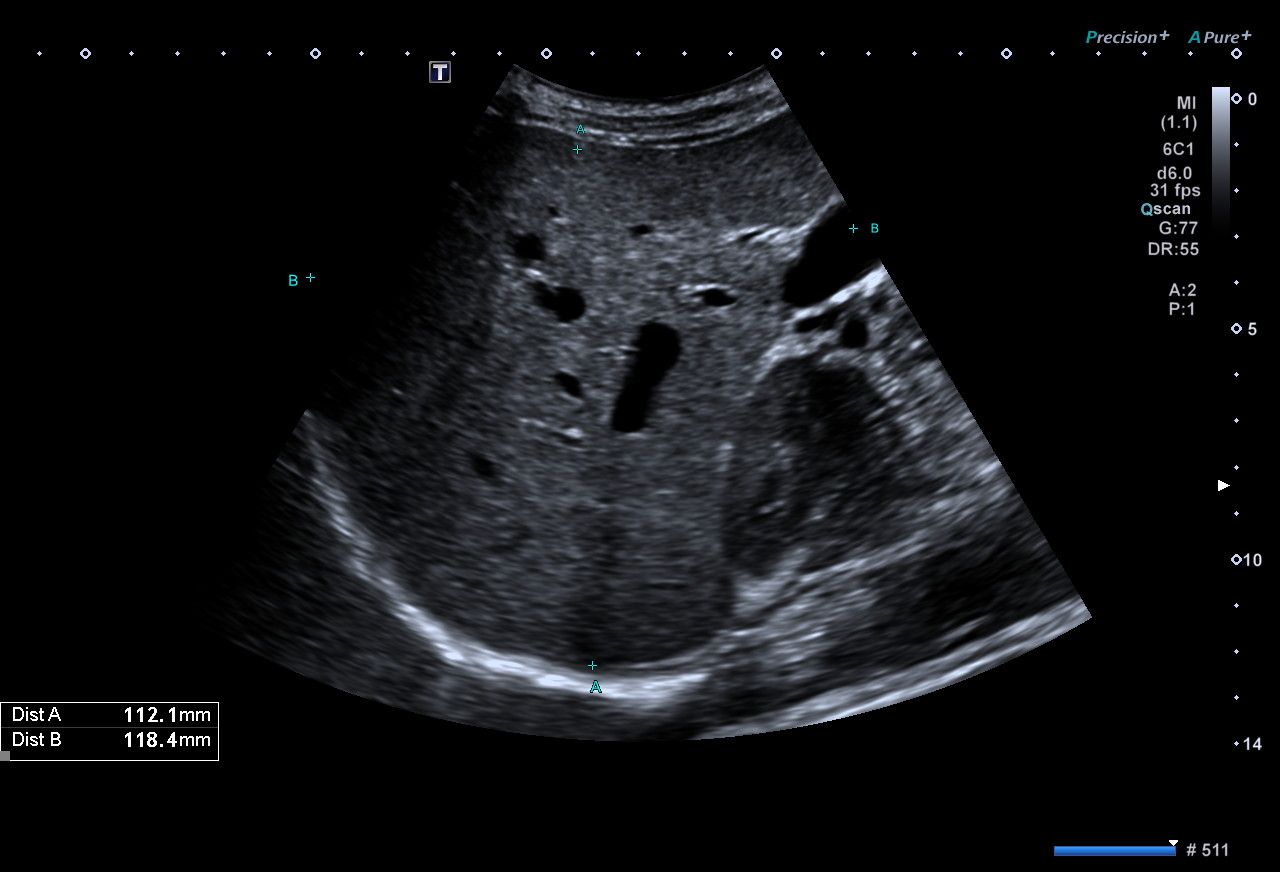
Spleen:
-
@BearWithMe
Hi, I can't help to interpret such ultrasound images (yet). All I see, if those measurements are done right, is that both your liver and spleen are indeed really small.
Is that a good thing and sign of extraordinarily good health? I don't know. Probably if I were your GP and only saw those ultrasound reports I'd throw in the towel and deem so.Earlier you mentioned chemically induced GI issues, what kind of chemicals might induce such symptoms?
Anything, really, especially if regeneration or lymphatic clearance are not up it. Emulsifiers, detergents, micro(nano)crystalline cellulose, NSAIDS, glucocorticoids, various other medications or caustic chemicals.
GABA powder and ensure adequate b12 + choline, to support forward peristaltis. Figure out what kind of pathogen colonized my digestive tract (if any) and then use targeted therapy to eradicate that pathogen, and/or use Camphoric acid as a non-specific treatment
That's what I'd aim at. If it's H. pylori that would be the most obvious and discernable cause.
Flowers of sulphur would only tackle lumen contents but e.g. no fluke in the biliary/pancreatic duct (which in rare very circumstances wouldn't excrete eggs in stool).monolaurin as an adjuvant therapy, to support the main antibiotic / antifungal?
I had looked into that and wasn't convinced by its selectivity against only some bacterial species. If it's anticandida/-fungal I would first want a semi-quantitative analysis of fungus in stool and still focus on the other drugs & biofilm- & membrane-breaking enzymes like hemicellulases.
GABA powder cures my insomnia within minutes of taking, btw.
Neat!
-
@CrumblingCookie Thank you so much.
I have found a lab that can test all pathogens you mentioned. Any other pathogens I should test? Aspergillus and Saccharomyces maybe? I suspect the pathogen in my gut might be producing ethanol
-
I'm eating 2500-3000 kcal, 350-450g of starch, every day, without an exception, since June 2023. I'm not physically active, walking from my workroom to bathroom is usually the only physical activity I engage in. Despite being in huge caloric surplus for very long time, I'm not gaining any body fat.
My stool looks like mostly undigested food. What I eat goes out without much change in appearance (or smell). Could it be that my body is slowing down / halting the motility, because it sense the food is not digested enough to move on to the next phase of digestion, but it is never digested enough to move on to the next phase of digestion? So it just sits there, waiting to be digested, but not being digested? Not sure if this is even possible?
-
@BearWithMe
Have a look into raising acetylcholine-dependent vagus-nerve regulation of intestinal motility and those esophagus-to-anus "rush waves" by replenishing with high-dose B5, along with alpha-GPC (or cholinebitartrate if you stand the fishy smell) and perhaps some R-ALA and thiamine to round it off wrt the pyruvate->acetate reaction by the PDH complex.
Should be similar in effect as but more fundamental than taking GABA powder.
Maybe that's a possible explanation for food not progressing through the GI system in an orderly fashion but staying in place for long times and with weird, nonproductive spasms/contractions until eventually more foods or liquids arrive to push it through those "static" sections. Which results in a skipping of those digestive sections and a symptoms complex of both lack of motility and diarrhea, maldigestion and malabsorption. All hypothetical!
Also, nicotine enhances the postsynaptic action of ACh through nicotinic ACh receptors. In the short term and if not overdone (because otherwise receptor densitiy will adapt). I suppose that's behind the infamous dump after a cigarette and coffee. -
@CrumblingCookie This makes a lot of sense. Thank you very much.
Almost all supplements cause rapid destruction of my teeth. They have the same effect (possibly even worse) when applied topically. B-Vitamins, choline, fat soluble vitamins, magnesium, zinc, gaba, iodised salt... I can't even use skin moisturizers because when I do, I'm losing teeth.
I can probably push through and take the supplements anyways but the toothache makes it very hard to eat. Also, I don't want to be toothless in my early 30s.
Maybe eradicating the pathogens in my gut first would help?
-
@BearWithMe
I don't know what to make of those teeth issues.
If you really have significant fat malabsorption then those fatty acids in the lumen will saponify with Ca and Mg, preventing uptake of both. Any extra metabolic stimulus may raise the requirements for those minerals, besides perhaps also generating more endogenous oxalic acid, thus dissolving bone/teeth. -
@CrumblingCookie Also makes a lot of sense.
Should I keep my fat intake as low as possible? How much calcium should I supplement?
I'm worried that too much calcium carbonate long term might contribute to gastroparesis. I can't digest milk, calcium carbonate is my only source of calcium
-
@BearWithMe
I think it's ideal to have about 200-300mg Ca per meal for absorption and for binding to dietary oxalic acid. Over the course of a day allegedly the average requirement is about 1200mg Ca.
Just do what's comfortable and makes sense to you.The Ca-carbonate will always neutralize some gastric acid.
You could get 80% L/R/+ lactic acid, dilute it down to 5% and use that every day to blend with your stash of Ca-carbonate to convert it to Ca-lactate. That won't further react with gastric acid and also provide some L-lactate as an energy source. And if mucosal skin works similarly as outer skin then lactate will stimulate cell renewal in the stomach and upper GI sections. -
@CrumblingCookie Oh, that's brilliant. I like this idea a lot. Thank you very much!