Log: Extremely Low Cholesterol, Low Copper, Ceruloplasmin, High DHEA-S - Chronic Fatigue For Years
-
@Sigma said in Log: Extremely Low Cholesterol, Low Copper, Ceruloplasmin, High DHEA-S - Chronic Fatigue For Years:
Another elephant in the room is the low copper and low ceruloplasmin which both have been deficient for years. I don’t know if this is true copper deficiency but I definitely at least have paradoxical deficiency where it seems like I have zero bioavailable copper. On my recent test, zinc also came back at over 800, which was more than a hundred points over the reference range.
I asked perplexity ai:
Copper becomes biounavailable in the body primarily due to insufficient binding proteins and mineral imbalances. Key factors include:
- Deficiencies in Copper-Binding Proteins
Ceruloplasmin and metallothionein are critical for transporting and stabilizing copper. Reduced adrenal gland function (common in chronic stress) impairs ceruloplasmin production.
Sluggish liver function further limits synthesis of these proteins, leaving copper unbound and prone to accumulating in tissues.
- Zinc and Mineral Deficiencies
Zinc deficiency disrupts the zinc-copper balance, allowing copper to accumulate in tissues. Causes include high stress, plant-based diets, and processed food consumption.
Manganese and other trace mineral deficiencies exacerbate copper dysregulation.
- Dietary and Environmental Factors
High estrogen levels (e.g., from hormonal birth control) increase copper retention, while sulfur-containing amino acids (found in eggs/meats) are needed for detox pathways.
Soil depletion and exposure to pesticides/copper sulfate reduce mineral intake or increase toxic copper exposure.
- Genetic and Metabolic Factors
Conditions like Wilson’s disease (rare) cause pathological copper accumulation.
Oxidative stress from biounavailable copper may deplete antioxidants, perpetuating dysfunction.
Consequence: Unbound copper circulates freely, causing oxidative damage and symptoms like fatigue, hormonal imbalances, and neurological issues.
And now, "how would zinc excess relate to copper deficiency?"
AI:
High zinc levels can reduce copper availability through antagonistic interactions and competitive absorption mechanisms:
- Absorption Competition
Zinc and copper share similar intestinal transporters (e.g., metallothionein). Excess zinc upregulates metallothionein, which binds copper and prevents its absorption, leading to excretion.
- Enzyme Disruption
Zinc overload inhibits copper-dependent enzymes, such as cytochrome c oxidase and superoxide dismutase (SOD), impairing copper’s roles in energy production and antioxidant defense.
- Hormonal and Metabolic Effects
Elevated zinc lowers copper retention, as shown in studies where 24 mg/day of zinc reduced serum copper levels despite adequate dietary copper intake.
Chronic zinc supplementation can induce secondary copper deficiency, linked to anemia, fatigue, and neurological issues.
Clinical Implications
Ideal zinc-to-copper ratio: ~8:1. Deviations (e.g., from supplements or zinc-rich diets) disrupt this balance, exacerbating inflammation, immune dysfunction, and oxidative stress.Symptoms of imbalance: Neurological decline, cardiovascular risks, and mood disorders due to disrupted dopamine/norepinephrine synthesis.
Management: Monitor zinc intake (avoid oversupplementation), ensure dietary copper sources (nuts, shellfish), and test serum levels to guide correction.
On low copper and low cholesterol:
Copper deficiency disrupts cholesterol metabolism through altered enzyme activity and lipoprotein oxidation, leading to hypercholesterolemia and increased cardiovascular risk. Key mechanisms include:
- Increased Cholesterol Biosynthesis
HMG-CoA reductase upregulation: Copper deficiency elevates hepatic glutathione (GSH), which stimulates HMG-CoA reductase—the rate-limiting enzyme in cholesterol synthesis. This drives excess cholesterol production, raising total plasma cholesterol levels.
Animal studies: Copper-deficient rodents show a >50% increase in total cholesterol and an 85–288% rise in HMG-CoA reductase activity.
- Lipoprotein Dysregulation
Atherogenic lipid profile: Copper deficiency increases triglycerides in LDL and VLDL particles while reducing HDL functionality. LDL/VLDL become more prone to oxidation due to decreased SOD1 activity and higher triglyceride content.
Impaired cholesterol efflux: Reduced lecithin:cholesterol acyltransferase (LCAT) activity in copper deficiency limits cholesterol esterification in HDL, hindering reverse cholesterol transport.
- Interplay with Cholesterol Homeostasis
Reciprocal regulation: Copper and cholesterol metabolism are inversely linked. High cholesterol diets reduce hepatic copper, while copper supplementation lowers total cholesterol and LDL in hypercholesterolemic patients.
APP processing: Copper deficiency promotes amyloidogenic processing of amyloid precursor protein (APP) in lipid rafts, potentially disrupting cholesterol feedback mechanisms mediated by Aβ peptides.
- Clinical Implications
Hypercholesterolemia: Marginal copper deficiency may underlie elevated cholesterol in ~40% of hypercholesterolemic patients, reversible with copper supplementation (e.g., 5 mg/day).
Oxidative stress: Copper-deficient LDL/VLDL are more susceptible to oxidation, accelerating atherosclerosis.
Conclusion: Copper deficiency drives hypercholesterolemia via HMG-CoA reductase activation and lipoprotein oxidation, contributing to ischemic heart disease. Restoring copper levels may normalize cholesterol profiles and reduce cardiovascular risk.
More specifically:
A combination of low copper, low ceruloplasmin, and low cholesterol is uncommon but may occur in specific contexts. Here’s the breakdown based on the search results:
- Copper and Ceruloplasmin Deficiency
Primary mechanism: Ceruloplasmin synthesis depends on copper availability. Low copper (e.g., dietary deficiency, malabsorption) reduces ceruloplasmin production, as copper is required for its enzymatic stability.
Genetic exceptions: Wilson’s disease (WD) typically involves high hepatic copper but paradoxically low serum ceruloplasmin due to ATP7B dysfunction. However, WD does not explain low copper levels.
- Low Cholesterol in Context
Peripheral vs. brain cholesterol: While copper deficiency usually increases peripheral cholesterol via HMG-CoA reductase upregulation, brain cholesterol synthesis is impaired in copper-deficient states (e.g., Menkes disease, cuprizone exposure), leading to demyelination and reduced brain cholesterol.
Wilson’s disease anomaly: In WD, hepatic copper overload correlates with hypocholesterolemia due to liver dysfunction impairing cholesterol synthesis/secretion. However, this involves high tissue copper, not systemic deficiency.
- Potential Scenarios for Low Copper, Ceruloplasmin, and Cholesterol
Advanced liver disease: Severe hepatic dysfunction (e.g., cirrhosis) may reduce ceruloplasmin synthesis and cholesterol production, even with normal copper intake.
Combined metabolic defects: Rare genetic disorders affecting both copper transport (e.g., Menkes-like syndromes) and cholesterol biosynthesis pathways could theoretically lower all three parameters, though this is not explicitly documented in the literature.
Conclusion: The triad of low copper, ceruloplasmin, and cholesterol is atypical. Possible explanations include severe hepatic dysfunction or niche neurological conditions impairing brain cholesterol synthesis. Wilson’s disease (high copper, low ceruloplasmin) or isolated copper deficiency (low ceruloplasmin, high cholesterol) do not fully align with this profile. Clinical evaluation for liver pathology or rare genetic/metabolic disorders is warranted.
Trying to tie things together with low DHEA-s, so I asked again:
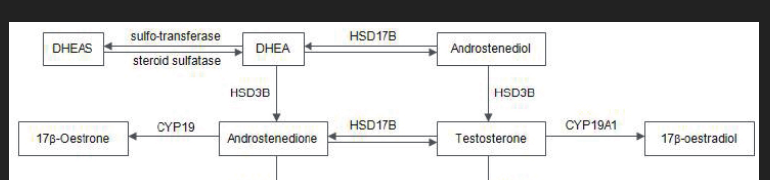
The relationship between low copper, low cholesterol, low ceruloplasmin, and high DHEA-S involves interconnected hormonal and metabolic pathways, though direct causation is not fully established. Here’s the synthesis based on the search results:
- Copper Deficiency and Ceruloplasmin
Ceruloplasmin dependency: Ceruloplasmin, a copper-binding protein, requires adequate copper for synthesis. Low copper levels reduce ceruloplasmin production, as seen in dietary copper deficiency or malabsorption disorders.
Hormonal feedback: Copper deficiency in rats decreases serum DHEA by ~50%, suggesting copper’s role in adrenal steroidogenesis. However, this contrasts with elevated DHEA-S in humans, implying species-specific or compensatory mechanisms.
- Cholesterol and Steroidogenesis
Cholesterol as a precursor: Cholesterol is essential for synthesizing steroid hormones, including DHEA-S. While copper deficiency typically raises peripheral cholesterol via HMG-CoA reductase activation, low cholesterol in this context may reflect:
Impaired synthesis: Severe liver dysfunction (e.g., Wilson’s disease) reduces cholesterol production, though this usually involves high hepatic copper, not deficiency.
Increased utilization: Enhanced conversion of cholesterol to DHEA-S (via CYP11A1 upregulation) could deplete cholesterol stores.
- DHEA-S Elevation Mechanisms
Enzymatic stimulation: DHEA-S enhances CYP11A1 activity, increasing cholesterol-to-pregnenolone conversion by 26%. This could deplete cholesterol reserves while elevating DHEA-S output.
Adrenal compensation: Low copper may trigger adrenal hyperactivity to maintain steroidogenesis, paradoxically raising DHEA-S despite systemic deficiencies.
- Contradictions and Gaps
Copper-DHEA-S paradox: While rat studies show copper deficiency lowers DHEA, human data on DHEA-S in copper deficiency are lacking. Elevated DHEA-S might reflect:
Stress response: Chronic stress (common in copper deficiency) increases adrenal DHEA-S secretion.
Assay interference: Cross-reactivity in DHEA-S measurements with other sulfated steroids in copper-deficient states.
Conclusion
The triad of low copper, ceruloplasmin, and cholesterol with high DHEA-S suggests a complex interplay:Copper deficiency impairs ceruloplasmin synthesis and may disrupt adrenal steroid balance.
Compensatory upregulation of CYP11A1 (potentially via DHEA-S) could drive cholesterol utilization for steroidogenesis, lowering serum cholesterol while elevating DHEA-S.
Clinical evaluation for adrenal dysfunction, liver pathology, or assay artifacts is warranted, as this pattern defies typical copper-deficiency phenotypes.
Note: Direct evidence linking these parameters is limited, and mechanisms remain speculative. Further research is needed to clarify causal relationships.
I don't know if you've checked this stuff it out, it may be old news to you. The AI gives somewhat contradictory findings, but also says these deficiencies are atypical and point towards Wilson's disease, though that is genetic.
Wilson's Disease, cholesterol, and low copper:
Wilson’s disease (WD), caused by mutations in the ATP7B gene, disrupts copper metabolism and leads to hypocholesterolemia (low cholesterol levels) primarily through hepatic dysfunction and altered lipid metabolism. Key mechanisms include:
- Hepatic Injury and Cholesterol Synthesis
Impaired liver function: Copper accumulation damages hepatocytes, reducing the liver’s capacity to synthesize and secrete cholesterol. This is evident in WD patients with hepatic symptoms, who show significantly lower total cholesterol compared to asymptomatic individuals.
Downregulated cholesterogenic genes: In animal models (e.g., Atp7b−/− mice), hepatic copper overload suppresses genes involved in cholesterol biosynthesis (e.g., HMG-CoA reductase) and nuclear receptors like LXR and FXR, which regulate lipid metabolism.
- Lipoprotein Alterations
Reduced VLDL cholesterol: Studies in WD animal models show a 3.6-fold decrease in VLDL-cholesterol due to impaired hepatic lipoprotein assembly and secretion.
HDL/LDL changes: Human studies report variable effects, with some WD patients showing lower HDL or LDL, though these trends are less consistent than total cholesterol reductions.
- Clinical Observations
Hepatic vs. neurologic presentation: Patients with hepatic involvement exhibit more pronounced hypocholesterolemia, correlating with elevated liver enzymes (ALT/AST) and reduced albumin.
Treatment effects: Zinc therapy in WD patients may further lower cholesterol, though human studies show mixed results compared to animal models.
- Species-Specific Differences
Animal models: Rodent WD (e.g., LEC rats) consistently show hypocholesterolemia and hypotriglyceridemia, while human WD patients may retain normal triglyceride levels despite low cholesterol.
Conclusion: Wilson’s disease reduces serum cholesterol primarily due to copper-induced liver damage impairing cholesterol synthesis and lipoprotein secretion. The severity correlates with hepatic involvement, distinguishing it from neurologic-predominant cases
On what minerals may help liver function:
Conclusion: Zinc, selenium, molybdenum, magnesium, and manganese support liver repair and hormone regulation through overlapping antioxidant and enzymatic roles. Their functions often complement copper’s involvement in SOD and ceruloplasmin activity, making them critical in holistic liver-hormone health strategies.
On copper, zinc, and Metallothionein:
Zinc tends to accumulate in the body when ceruloplasmin levels are low due to the inverse relationship between copper and zinc and their competitive interactions in absorption and metabolism. Key mechanisms include:
-
Competitive Binding to Metallothionein
Zinc and copper compete for binding sites on metallothionein, a protein in the small intestine that regulates mineral absorption. When ceruloplasmin is low (indicating copper deficiency), excess zinc increases metallothionein production, which preferentially binds copper over zinc. However, this leads to copper being trapped and excreted, allowing zinc levels to rise. -
Inverse Relationship Between Copper and Zinc
Copper and zinc have an antagonistic relationship in the body. When copper levels are low (as reflected by reduced ceruloplasmin), zinc levels tend to increase because their metabolic pathways are interlinked. For example, low ceruloplasmin reduces copper’s ability to regulate zinc metabolism, leading to zinc accumulation. -
Reduced Copper Utilization
Ceruloplasmin is a major carrier of copper in the bloodstream and plays a role in iron metabolism. Low ceruloplasmin impairs copper transport and utilization, creating an imbalance that favors zinc accumulation. -
Hormonal and Metabolic Effects
Zinc is involved in numerous enzymatic functions (e.g., antioxidant activity via superoxide dismutase). When ceruloplasmin is low, oxidative stress may increase, prompting the body to mobilize more zinc as part of its antioxidant defense system.
Conclusion: Low ceruloplasmin disrupts copper metabolism, leading to competitive absorption dynamics that favor zinc retention. This imbalance highlights the need for careful monitoring of both minerals in conditions affecting liver function or systemic inflammation.
Not sure if this is the or a goal, but, on "how to increase ceruloplasmin production:"
To increase ceruloplasmin levels, focus on optimizing copper availability, supporting liver function, and addressing nutritional/hormonal factors. Here’s a structured approach based on the search results:
- Address Copper Status
Ensure adequate copper intake: Dietary sources (shellfish, organ meats, nuts) or supplements (if deficient) can boost copper, which is essential for ceruloplasmin synthesis.
Avoid excessive zinc: High zinc intake (>50 mg/day) competes with copper absorption, reducing ceruloplasmin production.
- Key Nutrients to Support Ceruloplasmin
Sulfur-containing amino acids:
Cysteine/Methionine: Found in eggs, poultry, and legumes; cysteine provides sulfur for ceruloplasmin’s enzymatic activity.
N-Acetyl Cysteine (NAC): Enhances cysteine availability, promoting ceruloplasmin activity.
Vitamins:
Vitamin A / Retinoic acid: Stimulates ceruloplasmin synthesis in the liver (supported by rodent studies).
Vitamin C : Increases ceruloplasmin production and supports copper absorption.
Vitamin E: Enhances ceruloplasmin activity by reducing oxidative stress.
- Hormonal and Metabolic Support
Estrogen: Increases ceruloplasmin synthesis in the liver (e.g., birth control pills, hormone therapy).
Liver health: Treat inflammation, infections, or liver disease (e.g., Wilson’s disease) to restore ceruloplasmin production.
- Avoid Inhibitors
Medications: Anti-seizure drugs (e.g., valproic acid) may elevate ceruloplasmin but should not be used solely for this purpose.
Inflammation: Chronic inflammation increases ceruloplasmin as an acute-phase reactant, but resolving underlying inflammation is critical.
- Clinical Considerations
Test copper and zinc levels: Low ceruloplasmin may reflect copper deficiency or zinc excess.
Genetic screening: Rule out Wilson’s disease (low ceruloplasmin with high hepatic copper).
Summary: Increase ceruloplasmin by ensuring sufficient copper intake, supporting sulfur metabolism (via NAC/cysteine), and optimizing vitamins A/C/E. Address hormonal imbalances (estrogen) and liver health while avoiding zinc overload. Always consult a healthcare provider to address underlying conditions.
Again, this is an AI so I'd look into these patterns in more detail to verify the information.
-
@Corngold Appreciate you trying to find something but I know all this already.
I've been researching this for close to 10 years, been utilizing AI also since last year.
Biggest thing is how to increase ceruloplasmin, cholesterol, androgens and shift the system from stress, cortisol, catabolic towards anabolism, low stress etc.
Basically how to make copper bio available?
It could be toxic copper hiding in tissues. It could be plain copper deficiency. However copper makes me wired and feel crazy.
So I still lean towards the first solution.
Only question is how do I break this cycle?
-
@Sigma
I remember your account, not sure about the cholesterol part (curious what could have helped elevate it again, or what could have stopped lowering it?)
but for the copper partyou showed low ceruloplasmin, ceruloplasmin gets created in the liver in response to copper in the tissue. so its 1 way to tell if copper overloaded for some reason (in a probably uncommon situation) or not, because if copper is high in liver generally ceruloplasmin shouldn't be low (some exceptions like wilsons where they cant put the copper into the protein so it degrades, But you also didn't have elevated liver enzymes at the same time so didn't show damage which should be there if there's an overload problem doing significant damage - doesnt give me a reason to think overload)
ray peat wrote in his book copper is vulnerable as we age and tends to be lower with iron ratio going up. and the lower copper causing some aging outcomes. damaging in high amounts or to vulnerable gut but cells / mitochondria cant function properly without enough, cytochrome c needs it
and u have high zinc-copper ratio.
and lung / breathing problems without iron deficiency also points to low copper.
and both copper measures showing low.
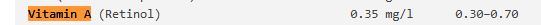
from what i can see it points to low in both blood & tissue. If i was in your situation i would stop all extra zinc if u haven't yetIf your vitamin A is too low atp7b / ceruloplasmin gets impaired. when you take cells similar to wilson's and add vitamin A it helps raise ceruloplasmin again.
Do you get much vitamin A in diet? avoiding either / not getting enough can lead to problems
https://pmc.ncbi.nlm.nih.gov/articles/PMC9616579/#sec2
Vitamin A also key in testosterone production so fits twice
https://pmc.ncbi.nlm.nih.gov/articles/PMC6216111/
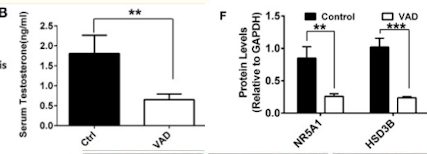
And far as DHEA with low test, (wasnt in 2022 functionally by DHT level)
With vitamin A too low HSD3b goes down. hsd3b = dhea -> androstenedione.& you had low end vit A before, but not deficiency.
At that time 2022 your DHT levels were up in that range. Test wasnt the best but not crashed in the range like now and DHT is more potent. Cholesterol low, copper low.
So that doesn't fit with copper, unless you were avoiding copper or on low copper diet at that time with the vit A unable to help increase ceruloplasmin that needs enough copper to be bound.
Your test is low now with cholesterol higher (less conversion maybe).
Both times your cholesterol was in the 80s your androgens weren't low (higher conversion maybe).
I'm thinking maybe the difference is vit A going into sufficiency at least 1 of the times, maybe both but not measured. If you were restricting / on low copper before
How much copper & vit a do you get?
If low increasing vit A might be worth a try to see if fixes some things if get enough copper in diet simultaneously (nothing wild) , (and arent taking supplements to deplete e.g 100s of milligrams of flavanoids with copper vulnerable to depletion by them). (and without the extra zinc). i wouldnt get from carotene sources just in case conversion issue. -
So from age 13-18 you were not in a nourished state but a stressed one?
That age range is paramount for development
Stay the course
If you’re overtraining or doing anything else that keeps you in a stressed metabolic state-
You need to stop“A stressed organism cannot heal”- paraphrasing
Looks like you are drinking too much liquid imo as well
Hard on digestion imeI will add I only skimmed your post
But you get my big idea hopefullyAddendum: oh dear. I just read more of your post. Yeah. You need to really step back and look at basics. Much to say but not enough time here….
-
@cs3000 Thanks for replying bro. I also studied your posts on the old forum. You were doing pretty good with pregnenolone, no?
Yeah. What you are saying seems right.
Vitamin A seems to be a key player for me. Whenever I researched ceruloplasmin, vitamin A obviously popped up.
I actually had one of my craziest experiences a few years ago after supplementing 10k vit A. I had throw up a bunch of bile about half an hour after taking it and then afterwards I was feeling the most low cortisol, androgenic state I have had in a long time.
A few weeks ago I also supped vit A a few times. It seemed to have some anti stress effects but just after the whole anti vit A propaganda, I got some worries about supplementing with it.
@cs3000 said in Log: Extremely Low Cholesterol, Low Copper, Ceruloplasmin, High DHEA-S - Chronic Fatigue For Years:
Do you get much vitamin A in diet? avoiding either / not getting enough can lead to problems
I am definitely not avoiding it. I never really went low A like the lowtoxin guys and these days my diet has sufficient. Same for copper. The only thing is I am also using a lot of vit A antagonists maybe. Like all the zinc uses up vit A etc.
I actually seem to have a weird problem where I have too much bile production, or my liver is too lean. That's how it feels like at least. I will drink a coffee and have the craziest bile and feeling too much on edge. Could be the opposite of the lowtoxin / low A guys who all struggle with high cholesterol, high vit A etc.
@cs3000 said in Log: Extremely Low Cholesterol, Low Copper, Ceruloplasmin, High DHEA-S - Chronic Fatigue For Years:
And far as DHEA with low test, (wasnt in 2022 functionally by DHT level)
With vitamin A too low HSD3b goes down. hsd3b = dhea -> androstenedione.This is very interesting. Could be like you say that the low A makes the DHEA-S pool and not convert into androgens.
Also are you saying its impossible to have low testosterone functionally with my DHT level at that time? I wonder what it is now.
I've been thinking and researching a lot and thinking again about trialing pregnenolone and even progesterone. I've been uploading all my data and experiences to ChatGPT and he also said prog could be especially helpful in healing my brain and correcting neurosteroids/GABA sensitivity.
The reason I am thinking about prog is because of women with PCOS who have a messed up hormonal profile with high DHEA-S seem to have an issue with high estrogen and benefit from prog to calm the adrenals and flush out the estrogen. Classic Ray Peat fashion.
I was thinking maybe this could also help flushing estrogen out of tissues for me and then potentially improving ceruloplasmin and copper. Since ceruloplasmin also is estrogen dependent to an extent.
But I am worried about suppressing androgens even further.
Do you think it is at all possible that this is some kind of vit A toxicity. When I was young like I said in my post I used to eat 4-8 eggs a day, lots and lots of milk and dairy, lots of meat. And still I was feeling extremely low androgens back then, and felt like I was overloading my liver. That's the only thing that makes me worried about vit A.
Also ... if you want to see more labs and some more experiences, there is a lot more going on on the OG forum. Just got diagnosed with some weird sleep apnea.
-
silicon raises ceruloplasmin and lessens negative effect of copper deficiency in rats
https://www.sciencedirect.com/science/article/abs/pii/095528639090086Z
-
@eduardo-crispino Thats actually something that I wanted to try for a while. Read about silica and copper for a while. Didn't know it also actually raised cerulo.
-
@Sigma well here is a list of silicon rich foods:
- clausthaler original / classic beer (not the IPA) 330ml 0.5%abv 11mg silicon with highest bioavailability of any studied foods, matches the MMST supplement form and much higher bioavailability than even the BioSil supplements . this beer is also municipally added fluoride free and only uses hop extract and not a significant amount of hops in the brewing, so possibly not very estrogenic and I have read on rpf from a user that maybe beer is more progestognenic than estrogenic. most if not all beers will have silicon but this is the only confirmed beer ive seen showing silicon content amount
-green / French beans , second highest bioavailability tested. these are the types of beans you'd probably cook not eat raw. not talking about snap peas etc
-cucumber with skin on, the wartier and knottier the skin the better
-oatmeal, especially oat bran
-various whole grains and rices
-more incidental stuff like pineapple
-bananas have some decent amounts but apparently barely bioavailable
"bioavailability" in the study I've seen is measured by determining silicon content of the food then measuring how much comes out in urine. if a lot comes out in urine they call it "high bioavailability" because that means more is making it to the blood and not just passing through the digestive system unabsorbed and coming out as poop. just logically this method of determination might not be correct because maybe foods that are apparently low bioavailbility measurement via this method have silicon that is being uptaken to cells better so less is coming out in urine.
-
-
@cs3000 Can you elaborate on these studies bro?
I still kinda feel like the copper might be stuck in tissues.
I took 2mg today and I feel much more triggered, irritable.
I also have been taking progesterone here and there over the last week and I am not sure about it but in a way seems like it could be beneficial.
I asked chatgpt and progesterone can't convert into dhea or cortisol so it seems much safer than preg which actually can convert into dhea and this seems like exactly what happens when I take it. I get more stressed. On the prog, it doesnt seem to happen but again I am still unsure if I like the overall effect.
Also, vitamin A. On paper it should make sense. Raise ceruloplasmin, raise cholesterol and steroid hormones? Is there any form you recommend?
-
@Sigma you said somewhere you have issues with your trachea collapsing or something right causing interrupted sleep ,
those studies show copper plays a key role in elastins structure enables it to create proper elasticity, But it needs ceruloplasmin to do thatwith dysfunctional elastin breathing problems can happen (usually the lung e.g chronic shortness of breath)
but trachea is also elastic tissue needs proper elastin function for keeping its structure, lysyl oxidase to cross link elastin well (so your problem there maybe fits with your low ceruloplasmin)
but if your baseline vitamin A and copper intake has been good for a while changing diet there might be irrelevant idk. some people dont convert carotene to vit A well though
In conclusion, elastic system fibers are one of the extracellular matrix´s components concerning the trachea.
These fibers seem to give the trachea the capacity to increase in length and diameter, and also are essential to its elastic recoilmaybe best not to take supplements unless theres an absorption issue needing high amounts, its easy to overdo them and can cause problems,
that making u irritable is probably more dopamine -> noradrenaline conversion, too much at once.
and u might absorb even more than usual because of being low in it, plus you get it all hitting at once that way instead of extracting with food combined with other nutrients
and taking copper alone without getting some foundational vitamin a for ceruloplasmin might not be great idea idk the minimum needed, probably not much.so maybe better sticking to food for testing if you notice a benefit or not
can get both from a small amount of measured raw weight 8g beef liver (~1mg copper + a few thousand IU vit A which is a mix of retinyl and retinol)
can add a little chocolate if needed. i dont think theres need to go over 2000iu - 5000iu vit A for general intake, 10,000iu+ can cause problems
https://www.cambridge.org/core/services/aop-cambridge-core/content/view/403AC96660C617812248DBBB9E90E538/S0007114596000979a.pdf/interactions_in_indices_of_vitamin_a_zinc_and_copper_status_when_these_nutrients_are_fed_to_rats_at_adequate_and_increased_levels.pdf
shows vitamin A gives dose dependant increase of ceruloplasmin. but you dont need those extremes to raise it
5000iu might raise it by 5 days , with some baseline copper intake
https://therootcauseprotocol.com/wp-content/uploads/2024/05/Induction-of-Ceruloplasmin-Synthesis-by-Retinoic-Acid-in-Rats-Influence-of-Dietary-Copper-and-Vitamin-A-Status.pdf
i'd avoid zinc supplements,
idk what a good timeframe would be for testing if its effective for the trachea thing or its something else. guessing maybe 3 weeks idk. https://pubmed.ncbi.nlm.nih.gov/6217893/ can add intakes up on cronometer -
Apart from supplements, have you tried including well-tolerated green leafy vegetables, like asparagus or kale? It is often overlooked in the peat-sphere, but can be very helpful. Asparagus for example lowers excess ammonia, which often is a culprit for fatigue.