@Wildflower I agree with you completely. That's great to hear about your recent recovery! With which type of thyroid did you self-treat (T3/T4, T3, NDT), and at what dosage? Did you encounter any setbacks in the course of your self-treatment?
Posts made by banquos-ghost
-
RE: Normal Reference Ranges of Serum TSHposted in Literature Review
-
RE: Normal Reference Ranges of Serum TSHposted in Literature Review
Getting the right diagnosis can be frustrating for so many hypothyroidic patients because THIS is what they're faced with when consulting an endocrinologist:
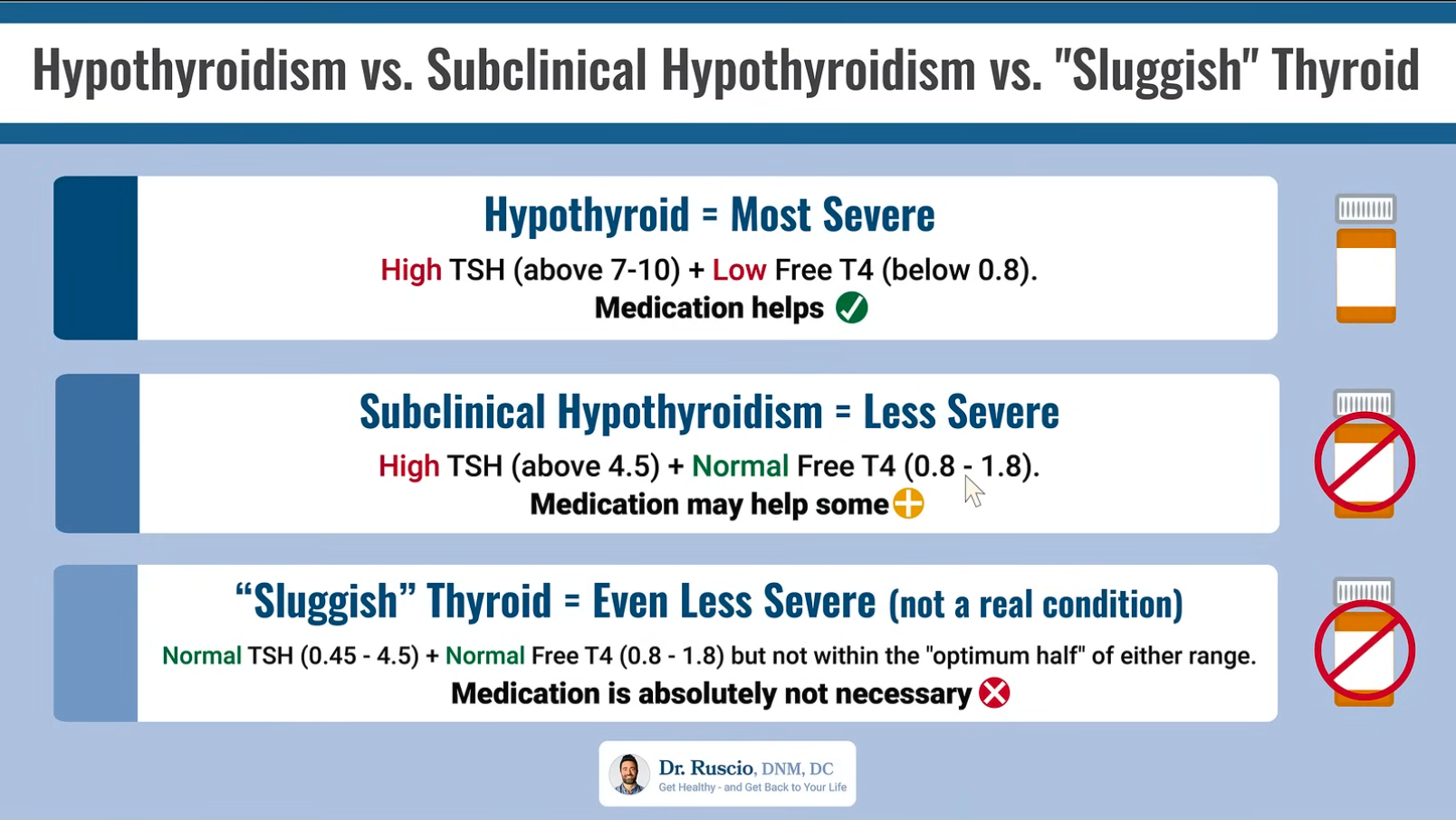
Medication is not really considered until TSH reaches dangerously high levels; T3 levels are not even considered when making the diagnosis, as if thyroid conversion is never an issue; and T4 levels are regarded as the sole marker of glandular production.
The creator of the video, from which the above chart is copied, says:
"[The most severe case is] a high TSH paired with a low free T4, according to the conventional lab ranges, not what your doctor may alter, using these different contemporary ranges, which are not correct."
"You really don't get into a position where you'll benefit from thyroid hormone, where you're considered hypothyroid, until your TSH gets somewhere above 7-10. . . . And we have pretty compelling data that answer this question: People in this subclinical range [TSH of 4.5-10] do not seem to have problems, they don't have more symptoms, and they certainly do not seem to benefit from thyroid hormone replacement therapy."
In such cases as these, where the endocrinologist is not the least bit willing to consider unconventional views, it's best to start looking for a new healthcare provider.
And of course—here's the kicker—the creator goes on to offer a $199 online course on how to manage thyroid symptoms. Yes, an online course.
-
RE: Chronic tinnitus?posted in Not Medical Advice
@Orindere In my experience, gut issues have directly caused my chronic tinnitus. This is because an intestinal infection increases circulating levels of pro-inflammatory cytokines, which are implicated in tinnitus. And I've noticed that when my digestion function speeds up, my tinnitus quiets down.
-
Thyroid Therapy Success Storiesposted in Bioenergetics Discussion
This a thread for forum users to share their success stories with thyroid therapy. Some important data to provide:
- Conditions and symptoms being treated
- Form, dosage, duration, and timeline of treatment
- Bloodwork and biometrics before, during, and after treatment
- Response to various types and sources of thyroid medication
- Supplements and dietary changes to support thyroid conversion and non-thyroidal endocrine health
-
RE: Trying out "T3 only" therapy -Wilson Protocolposted in Case Studies
@linx Have you ever tried combination T3/T4 therapy? Over what timeline have you worked up to 87.5mcg T3 daily?
-
Normal Reference Ranges of Serum TSHposted in Literature Review
Ray Peat said in "TSH, Temperature, Pulse Rate, and Other Indicators of Hypothyroidism":
"Over a period of several years, I never saw a person whose TSH was over 2 microIU/ml who was comfortably healthy, and I formed the impression that the normal, or healthy, quantity was probably something less than 1.0."
Xing et al. said in "Factors influencing the reference interval of thyroid‐stimulating hormone in healthy adults: A systematic review and meta‐analysis (2021)":
"Some reports define the lower limit of TSH as 0.2–0.4 mU/L and the upper limit as 4.0–5.0 mU/L, but a much lower upper limit of TSH has previously been suggested based on large population studies. The American Association of Clinical Endocrinologist recommended to decrease the upper limit of TSH to 3.0 mU/L. Many experts even suggest that the upper limit of the range be further reduced to 2.5 mIU/L."
"The results [of this meta-analysis] showed a higher TSH concentration in females than in males in most regions. Estrogen is an important factor affecting the TSH concentration. Low estrogen may cause hypothyroidism and then lead to an increased TSH concentration. Postmenopausal women were the typical group, and the TSH concentration increased significantly. This may be one of the reasons why TSH is generally higher in females than in males."
Ah yes, estrogen deficiency is the main culprit behind higher TSH levels in females.
"Surks et al reported that the 97.5 percentile of TSH increased from 3.56 mIU/L in the 20–29 years old group to 7.49 mIU/L in the over 80 years old group. In this study, the TSH concentration also increased with age. Some researchers have suggested that the progressive increase in the TSH concentration with ageing could be due to an enhancement in the prevalence of acquired autoimmune thyroid disease and an increase in anti‐thyroid antibodies."
"Guan et al suggested that it was necessary to consider iodine intake when establishing the TSH reference interval. Their study was conducted in Panshan, Zhangwu and Huanghua, regions with mildly deficient, more than adequate and excessive iodine intake, respectively, and the mean levels of TSH in Panshan, Zhangwu and Huanghua were 1.15, 1.28 and 1.93 mIU/L, respectively."
Biondi said in "The Normal TSH Reference Range: What Has Changed in the Last Decade? (2013)":
"An upper limit of the normal TSH range of 2 mIU/L and a lower limit of 0.4 mIU/L have been associated with a lower incidence of a progressively more deranged TSH value than other TSH values within the reference range [of 0.45 and 4.12 mIU/L]."
"Subsequent findings confirmed that ethnicity, iodine intake, gender, age, and body mass index can influence the reference range of serum TSH. In fact, the normal TSH upper limit was lower in African Americans (3.6 mIU/L) than in Mexican Americans or Caucasians (4.2 mIU/L). Reanalysis of these data 5 years later showed that the upper limit of normal serum TSH at the 97.5th percentile was 3.5 mIU/L in individuals 20–29 years old, 4.5 mIU/L in those 50–59 years old, and 7.5 mIU/L in those older than 80 years"
"...if the upper and lower limits of normal for a third-generation TSH assay are not available, an upper limit of 4.12 mIU/L and a lower limit of 0.45 mIU/L should be considered in iodine-sufficient areas. The NACB recommendation to lower the upper limit of the TSH normal range to 2.5 mIU/L should be balanced with the health and economic impact of a reduced serum TSH range. In fact, about 20–26% of the population would be hypothyroid if the upper limit of the normal range is lowered to 2.5–3.0 mIU/L."
Broda Barnes would argue that this estimated incidence of hypothyroidism is still too low.
Kratzsch et al. said in "New reference intervals for thyrotropin and thyroid hormones based on National Academy of Clinical Biochemistry criteria and regular ultrasonography of the thyroid (2005)":
"If we used the 97.5th percentile as proposed by the NACB, we found a comparable upper TSH limit of 3.77 mIU/L for the constraint and 3.63 mIU/L for the whole group. These concentrations are considerably lower than the currently used upper reference limit of 4.2 mIU/L proposed by Roche Diagnostics and the 97.5th percentile of 4.1 mIU/L from the NHANES III study. On the other hand, our values are markedly higher than 2.12 mIU/L, which was the upper limit in the study of Völzke et al. Moreover, these values are also higher than the cutoff of 2.5 mIU/L that has been proposed recently by the NACB for distinguishing between euthyroidism and preclinical hypothyroidism."
-
RE: Thyroid Therapy for Chronic Digestive Issuesposted in Case Studies
@secondkelping Ruminant muscle meat (bison, beef, venison) is normally consumed at only one meal a day. Increased consumption of muscle meat of all kinds (poultry, etc.) has in the past provoked an inflammatory response and slowed my digestive process, so I try to limit that.
Gelatin is consumed in stews, often added to fish soup, and in the form of bone broth when available; glycine powder is added to milk on occasion. I think the balancing of BCAAs has provided some symptom relief over the last several months, and will be continued during and after thyroid therapy.
-
RE: Thyroid Therapy for Chronic Digestive Issuesposted in Case Studies
@brad My average morning body temperature is highly suggestive of hypothyroidism. Now, whether that's the cause of all my symptoms is still uncertain, but we'll find out soon.
Always frustrating that physicians proved entirely useless in arriving at this conclusion, but at least we have communities like this to rely on. Thanks for all you've done in advancing the bioenergetic movement!
-
RE: Thyroid Therapy for Chronic Digestive Issuesposted in Case Studies
@secondkelping Thank you for the comment; it gives me hope of recovery.
The carrot salad and mushrooms were eaten daily for ~4 months at the beginning of '23; no symptom relief was provided, though my movements were bulkier.
My diet is dialed-in at this point. It consists mainly of locally grown ruminant meat, raw milk, and produce, as well as a good deal of fresh seafood (I live on the coast).
The plan is this: Await arrival of Cynoplus and Cynomel, reread thyroid books (Barnes, McGavack), prepare for T3/T4 treatment protocol, administer thyroid and monitor symptoms.
-
RE: Topical Minoxidil: is it really that bad?posted in Not Medical Advice
@Chud You may be advised to start anti-androgen therapy (Finasteride, Dutasteride) to prevent loss of transplanted hairs. For obvious reasons any medication of that kind should be strictly avoided.
-
RE: Thyroid Therapy for Chronic Digestive Issuesposted in Case Studies
Thanks, @CO3. I'll read Danny's article.
-
Thyroid Therapy for Chronic Digestive Issuesposted in Case Studies
I, male aged 32, presented to my general practitioner 8 months ago with the following symptoms: fatigue, cognitive impairment, depression, muscle and joint soreness, cold intolerance and frigid extremities, indigestion, chronic constipation, abdominal distention and bloating, oral thrush, and biofilm elements present in stool. After a brief physical examination, she advised that I “eat more fiber” and continue to monitor my symptoms. Prior to this, all forms of dietary and lifestyle intervention had been tried.
Upon my request, she referred me to a gastroenterologist in my area, who, based on my digestive symptomology, prescribed antibiotics (Rifaximin) for empiric treatment of small intestine bacterial overgrowth. At a dosage of 550mg thrice daily for 14 days, the treatment provided no symptom relief. Antifungals (Nystatin) and antiparasitics (Ivermectin) were tried but also proved inefficacious. General bloodwork (comprehensive metabolic panel) conducted subsequent to treatment showed no abnormal levels.
Without medical supervision, I decided to undergo hormonal bloodwork, under the suspicion that I was hypothyroidic. The results, though within the reference ranges, have confirmed that:
- T4, Free: 1.44 ng/dL (Ref: 0.82-1.77)
- TSH: 3.7 uIU/mL (Ref: 0.45-4.5)
- Reverse T3, Serum: 19 ng/dL (Ref: 9.2-24.1)
- T3, Free: 2.6 pg/mL (Ref: 2-4.4)
(Additional bloodwork results can be provided upon request.)
Today, my diet is rich in pro-metabolic foods, I consume plenty of coffee and tea, live in a tropical region, exercise regularly with wife and friends, and get adequate daily sunlight. Since all my symptoms and bloodwork suggest hypothyroidism, and since I have been unresponsive to other interventions, I am preparing to supplement with thyroid-promoting minerals (e.g. iodine, selenium) and/or treat directly with thyroxine (T4)+triiodothyronine (T3) combination therapy. Going forward, I will update this log with dosage, duration, and efficacy of treatment, as well as with updated blood markers when those are tested.