My Protocol for Hypothyroidism + Starch/Fat sensitivity
-
@pittybitty I can confirm that this protocol is indeed healing! I’m basically doing this now, not without a lot of trial and error to get here. Fantastic run down for anyone to follow.
-
@pittybitty Nice, how many litres of milk and juice are you aging a day?
-
@GlucoseGal glad to hear that, made my day honestly

@Testiclies just the one of each, I am adding simple syrup to them now to up the calories
-
There is something pretty important I have overlooked.
Calcium heavy and sugar heavy diets both reduce gastric acid. Low gastric acid causes poor mineral and protein absorption. The undigested proteins then are fed on by nasty strains of bacteria, and low gastric acid allows far more pathogens to enter the digestive tract, leading to SIBO or gut dysbiosis.
Long term we can offset this with ample coffeine and protein rich foods, but short term we should take Betaine HCl (625mg with every meal) to restore gastric acid and recover from the dysbiosis/SIBO.
-
@pittybitty
Hi,
My analysis- “The symptoms suggest digestive insufficiency due to elevated adrenaline and low thyroid”.
=> Stress could indeed make the things worse.
A low thyroid could bring a lot of lacks but … - “You should not focus on that” (dysbiosis as the cause of a vulnerable gut).
- fighting against SIBO / SIFO requires energy.
- “likely make you even sicker in the process”.
=> Right. Killing overgrowth bacteria (SIBO) and fungus (candidiasis) induces a Herxheimer crisis (mainly from LPS toxins).
- “The focus should be on recovering digestive capabilities first”
=> Too late. Explanation follows. - “Afterwards the body should be able to heal from dysbiosis by itself, without further intervention”
=> You dream. Sorry to be cash. If you don’t change the behavior and the root of the problem, homeostasis won’t take place. The tipping point has been crossed.
And if you think you could repair the leaky gut with some appropriate supplements without getting rid of WGA and prolamins from wheat, it won’t happen.
Explanation: WGA (wheat lectin) and gluten prevents the gastric brush barrier from recovering / reestablishing itself. And if you combine this problem with sluggish bowel movements (MMC), you've hit the jackpot.
Edit: You recover during the night if you haven't abused too often.
Both WGA and glutelin are wheat proteins, they have different structures, functions, and impacts on health.
Note: You’re free to try to experiment but don’t wait too long:
The brain could be targeting the wrong thing (autoimmune disease) when faced with an intruder it cannot control. Too much low-grade inflammation. See Jaqueline Lagassée if you need convincing. Keep the mind open, please.
I can give a more explicit link if a reader wants it.
- “The symptoms suggest digestive insufficiency due to elevated adrenaline and low thyroid”.
-
I am fully healed now, no remaining symptoms. I can eat everything again, no longer need the NDT and have full energy throughout the day.
I am still eating as during the protocol, just removed some supplements and with more "cheating". Greatly increased amount of eggs since those seem to do the liver a lot of good. Tongue discoloration comes back when I cheat with too much starch but no actual rebounds.
I have updated the OP with all the details.
-
@LucH said in My Protocol for Hypothyroidism + Starch/Fat sensitivity:
See Jaqueline Lagassée if you need convincing. Keep the mind open, please.
I can give a more explicit link if a reader wants it.Please post link , I would gladly read more about it.
-
@LucH said in My Protocol for Hypothyroidism + Starch/Fat sensitivity:
WGA and glutelin
Could you share what would be example of your one time meal (breakfast or lunch ?
-
@Gardner said in My Protocol for Hypothyroidism + Starch/Fat sensitivity:
Please post link , I would gladly read more about it.
Sorry by advance, if I'm too long. Go to the end of the text if you want to avoid the presentation.
The Intestine as Conductor
Excerpts from the book "A Targeted Diet to Maintain or Restore Intestinal Health." Jacqueline LAGACÉ, Doctor. The best book on the market, well presented and explained, in language accessible to both the uninitiated and healthcare professionals (sources). Give this book to your doctor (€22–25) and/or leave a copy of this document in a laminated folder that you may have accidentally left on the corner of the table It will be your gift for the one who is willing to "listen." But don't get your hopes up too much: Sometimes you have to sow a seed before it germinates...
It will be your gift for the one who is willing to "listen." But don't get your hopes up too much: Sometimes you have to sow a seed before it germinates...

Hypotoxic Diet: What the science says
A targeted diet to preserve or recover a healthy gut. The pain-killing effect of a hypotoxic diet
Thirteen years after the death of Dr. Jean Seignalet, his pioneering work continues to make adherents as recent advances in scientific research confirm the key elements of his hypotoxic diet. Since the mid-1980s, we don’t count any longer the evidences that Dr. Seignalet's hypotoxic diet has allowed people to recover their health. On the other hand, opposition does not weaken because of the virtually sacred nature of wheat and corn and other related cereals (barley, rye, oats, kamut) as well as dairy products and the role they play as locomotives of the rich agro-food industry...
Indeed, in front of those who claim to have regained their health thanks to the withdrawal of pro-inflammatory foods as recommended by the hypotoxic diet of Dr. Seignalet, the "mass argument" of the opponents consists of affirming peremptorily: “This is not proven!”, «This is only a fad!" According to them, only those with celiac disease are right to avoid gluten, the sticky substance that causes the bread to swell and is the main cause of intolerance due to the wheat and cereals that are related to it.
The theory of Seignalet is basically based on the observation that our digestive enzymes are poorly adapted to the digestion of modern foods characterized by the excess of wheat cereals (wheat is found in the majority of food processed by the food industry), and mutated (genetically modified), by dairy products derived from animals raised under conditions not respecting their herbivorous nature, by animal protein cooked at high temperature and processed food.
Wheat and dairy products: foods that are difficult to digest
The inability of our digestive enzymes to perfectly digest these foods is now confirmed by numerous scientific works which have demonstrated that gluten constituents, the peptides called gliadins, resist the action of our digestive enzymes. It is now known that the resistance of gliadins to digestive enzymes is due to their very rigid cyclic structure consisting of several repeated associations of two amino acids, proline and glutamine. Four types of gliadins (named alpha, beta, gamma and omega) were identified, which showed that gliadin-alpha has more pronounced pathogenic effects than other gliadins. In fact, gliadin-alpha has a superior ability to activate the immune system in an exacerbated manner, as well as other pathogenic characteristics that can alter the normal behavior of cells.
Research has shown that animal milk caseins have a structure similar to that of gliadin-alpha, the same rigid cyclic structure consisting of associations between the proline and glutamine amino acids. Moreover, the caseins of animal milk have an immunological relationship with gliadin-alpha since the antibodies developed against this peptide also react with caseins of animal milk. We must also take into account the inability of our enzymes to digest perfectly many other modern foods: junk food (foods dietetically unhealthy because of their low nutritional value), animal proteins cooked at high temperatures giving rise to unattainably perfectly digested proteins, glycotoxins, as is also the case for many foods processed by the agri-food industry.
The hypotoxic diet against intestinal hyperpermeability
The second basic principle of the hypotoxic diet developed by Seignalet is based on the need to preserve the balance of intestinal flora, which is essential for maintaining health and the ability to avoid the development of chronic inflammatory diseases.
According to Seignalet, it’s the accumulation in the intestine of food that we are unable to digest properly which causes the imbalance of the intestinal flora. This waste promotes the development of pathogenic bacteria to the detriment of the so-called commensal or saprophytic bacteria, which will lead to excessive permeability of the intestinal mucosa; The latter will allow indigested food and microbial molecules to pass through (antigens coming from the carapace of dead bacteria which are also insufficiently degraded by our enzymes) into the blood and lymphatic circulation as well as in the tissues.
These molecules, because they are insufficiently digested, keep their immunogenicity capacity, enabling them to exacerbate the immune system and possibly trigger chronic inflammatory diseases according to the genetic predispositions of individuals. For example, at the onset of development of osteoarthritis following the accumulation of sensitizing foreign antigens, a silent inflammation (without conscious pain) at the articular level, which can last from 10 to 40 years, before it becomes symptomatic; in other words said, before the individual begins to feel pain and / or suffer from loss of function.
Evidence now demonstrates the accuracy of Seignalet's theory of the influence of food and microbial molecules on the establishment of hyperpermeability of the intestinal mucosa: studies have shown that certain molecules in the wall of bacteria, called LPS – LPS stands for lipopolysaccharides –, as well as gliadin-alpha, have a major impact on the intestinal mucosa production of zonulin proteins. Zonulins have the ability to unbalance epithelial cells from tight junctions of the intestinal mucosa which causes excessive permeability of the intestinal mucosa and promotes the development of chronic inflammatory diseases. The official recognition of Non-Celiacs Gluten Sensitive (NCGS) dates back to 1978. However, it is only since 2010 that significant groups of researchers have become interested in NCGS and that double-blind, placebo-controlled research demonstrated the reality of the NCGS phenomenon, that people with gluten sensitivity while non-celiac had significant health problems when consuming gluten at that time, while these problems ceased when the gluten was withdrawn from their diet. The term gluten sensitivity in non-celiacs has recently been replaced by the term wheat sensitivity because other wheat antigens may also cause food intolerance in non-celiacs.
Sensitivity to Wheat in Non-Celiacs: Symptoms of Syndrome
The wheat sensitivity syndrome in non-celiacs usually results in a combination of intra- and / or extra-intestinal symptoms. Possible extra-intestinal symptoms include headache and / or migraines, feeling foggy, chronic fatigue, joint and muscle pain, tingling or burning sensation at the extremities, numbness of the legs, arms and hands, eczema, anemia, depression and peripheral neuropathies (exacerbated sensitivity of small terminal nerve fibers). In addition, links are often demonstrated between NCWS syndrome, attention deficit disorder, neurological and neuropsychiatric disorders, including autism and schizophrenia.
This broad range of pathological manifestations suggests that many chronic inflammatory diseases may be classified with non-celiac wheat sensitivity diseases (NCWS), which should be expanded to account for the diversity of adverse reactions to food and microbial antigens that may cause chronic inflammatory diseases.
A theory demonstrated by metagenomics
The ultimate demonstration of the accuracy of Dr. Seignalet's theories has come thanks to new techniques of genetic analysis: microbial metagenomics coupled with computer databases. These gene analysis techniques, which have taken off from 2010 onwards, provide rapid and accurate information on the diversity and relative abundance of microorganisms present in a given environment as well as their structural and functional features (enzymes, virulence factors, antibiotic resistance genes, etc.).
These techniques have proven that we are hybrid beings inseparable from the bacteria we harbor on us and in us. More precisely, it is now demonstrated that the balanced functioning of the saprophytic bacteria that live in our intestines is essential for maintaining our health and even our survival.
The importance of a healthy microbiome
These studies have shown that environmental factors, including the food we eat 3 times a day 365 days a year, as well as our way of life, influence the composition and the activity of the intestinal microbiome.
In fact, the intestinal microbiome is now considered as an organ in its own right: it encompasses microbiota (the intestinal flora) and the ecological environment of the intestine constituted by its different cells (epithelial cells, associated immune cells, enteric neurons – or second brain –, secretory cells and muscle cells). When the equilibrium of the intestinal microbiome is disturbed, this imbalance is called dysbiosis; this means that the number and variety of the good commensal intestinal bacteria have been disrupted in parallel with the proliferation of pathogenic bacteria and / or even the transformation of commensal bacteria into harmful bacteria; at the same time a disturbance of the ecology of the whole intestine occurs, namely that of the associated immune system, of the second brain and of the other cells which constitute the intestinal microbiome as mentioned above. The present work clearly shows that chronic diseases develop when there is an imbalance in the intestinal microbiome, which strongly favors the development of chronic inflammatory diseases according to the genetic fragilities of the individuals.
It was by highlighting the importance of the bidirectional microbiota-intestine-brain axis as a communication and execution network that we were able to understand how and why the intestinal microbiome conditions and controls the whole functioning of our organism, including our behavior.
The current epidemic of chronic inflammatory diseases (arthritic diseases, diseases affecting the intestine, heart disease, type 2 diabetes, neurodegenerative diseases, cancers and others) illustrates well the influence of the intestinal microbiome in individuals affected by these diseases, while conditions in our environment deteriorate (inappropriate feeding, lack of exercise, pollution, etc.).
Dr. Jean Seignalet had seen right!
It must be acknowledged that Dr. Seignalet has accomplished a real visionary and precursor work in developing the hypotoxic diet and demonstrating its effectiveness on approximately 2,500 people with many chronic inflammatory diseases. The fact that the majority of actors involved in current scientific research recognize the fundamental role played by the balance and / or imbalance of the intestinal microbiome in the maintenance of health or the onset of chronic inflammatory diseases proves indisputably that Seignalet had seen right. Moreover, it has been recently established by several publications that the essential factor of the balance of the intestinal microbiome is based on our food choices, an essential element of the hypotoxic diet.
Jacqueline Lagacé.
Ph.D., (doctor of virology) professor-researcher specialized in immunology and microbiology, director of a research laboratory for 17 years, retired from the Faculty of Medicine, University of Montreal. Blog jacquelinelagace.net
Author's books:- The end of pain. How nutrition and diet can fight chronic disease, 2011.
- New book in October 2016 : Une alimentation ciblée pour préserver ou retrouver la santé de l’intestin. L’effet antidouleur d’une diète hypotoxique. 22 – 25 €.
*) Forum (In French, translator required) about the book J. Lagacé
http://mirzoune-ciboulette.forumactif.org/t767-une-alimentation-ciblee-pour-preserver-ou-retrouver-la-sante-de-lintestin-leffet-antidouleur-dune-diete-hypotoxique#7341*) Jacqueline Lagacé site
English version of the book: “End of the pain”. 2014
The End of Pain: How Diet Can Fight Chronic Inflammatory Desease
https://jacquelinelagace.net/livres/the-end-of-pain-how-diet-can-fight-chronic-inflammatory-disease/I can give a summary of Jean Seignalet's guidelines if wanted.
-
@Gardner said in My Protocol for Hypothyroidism + Starch/Fat sensitivity:
Could you share what would be example of your one time meal (breakfast or lunch ?
To avoid or to limit. I'm no longer avoiding gluten (I've followed the principles for 2 years, just to shut a door - backpain). Strictly. Now I try to limit it.
For breakfast:
2 fruits for carbs. + one Medjool date if too short.
one tsp coconut oil if not enough fat or to balance MUFA / PUFA.
one protein: +/ 50 g Gouda cheese or ham or 2 enhanced eggs (free range) (2x/wk)
If required: I add shredded coconut (very thin dried slices).
NB: Need to manage potassium and especially magnesium, when eating hard cheese or ham.For Midday lunch
A salad, with half an apple, dried olive fruits or macadamia, + one veggie (tomato, cucumber, radish, mango, tangelo, mandarin, strawberries, etc.).- one protein afterwards: duck, beef, coquelet (small poultry), shrimps, caille).
I often eat Greek yoghurt (150 ml) with cuts of a fruit or blueberries or strawberries) or soft white cheese (full fat => 8%) (natural fat) with 1.5 tsp coconut sugar, to get all the nutrient). In alternance. With a break to avoid the unbalance of the microbiome. One third of the time per type: yogurt, a kind of cottage cheese, nothing (abstinence)
-
@LucH why do you eat only 2 fruits, or only 1 datte, or only half an apple at once?
-
@water-fire said in My Protocol for Hypothyroidism + Starch/Fat sensitivity:
why do you eat only 2 fruits, or only 1 datte, or only half an apple at once?
I didn't.
According to my body, activity, age and needs, I target +/ 2200 K/cal. No problem if I obtain 80 % of my objectives (to avoid becoming orthorexist), or if I eat 500 K/cal. more than what I planned.
As I didn’t want to get insulin problems, like my grandmother and mother, I got informed on how to manage glycemia.
200 – 250 g sugars (800 – 1000 K /cal)
25 – 30 g fiber
8 – 1.2 g protein per Kg weight (75 kg target for 22.5 BMI) (1m82 High)
=> 60 – 90 g protein.
30 % fat target (20 – 40 % is ok). Half from SFA
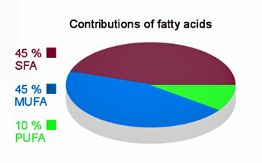
=> 45% SFA / AGS, 45 % MUFA / AGMI, 5-10 % PUFA / AGPI. Now 10 g maxi PUFA; 6 g target (1.5 g W3 and 4.5 g W6).
So it could give the following meals
500 - 600 for breakfast
700 – 900 K/cal. for lunch and evening meal
150 – 250 Kcal for a snack.
I try to limit carbs to 50 g at the breakfast, most of the time. The glycemia of the first meal is going to impact the whole day (prevention for insulin spike). See Jessie Inaupsché for details, even if she is not the new bible
When I eat 2 medium potatoes, I reach 80 g carbs but I dress my carbs: I add butter, one egg and veggies (broccoli flowers or frozen spinach or carrot). Some Ca or Mg / K is required when eating spinach (660 mg oxalate per 100 g) (prevention lithiasis / Kidney stones).
If you don’t want to “manage”, keep in mind, you should first begin with veggies, meat with fat afterwards, and carbs at the end, when dealing with glycemia problems.
Please, don’t tell me you don’t want to bother because you manage well when eating manufactured food (pizza, risotto or fried food). Fine for you… -
@LucH said in My Protocol for Hypothyroidism + Starch/Fat sensitivity:
@Gardner said in My Protocol for Hypothyroidism + Starch/Fat sensitivity:
Could you share what would be example of your one time meal (breakfast or lunch ?
To avoid or to limit. I'm no longer avoiding gluten (I've followed the principles for 2 years, just to shut a door - backpain). Strictly. Now I try to limit it.
For breakfast:
2 fruits for carbs. + one Medjool date if too short.
one tsp coconut oil if not enough fat or to balance MUFA / PUFA.
one protein: +/ 50 g Gouda cheese or ham or 2 enhanced eggs (free range) (2x/wk)
If required: I add shredded coconut (very thin dried slices).
NB: Need to manage potassium and especially magnesium, when eating hard cheese or ham.For Midday lunch
A salad, with half an apple, dried olive fruits or macadamia, + one veggie (tomato, cucumber, radish, mango, tangelo, mandarin, strawberries, etc.).- one protein afterwards: duck, beef, coquelet (small poultry), shrimps, caille).
I often eat Greek yoghurt (150 ml) with cuts of a fruit or blueberries or strawberries) or soft white cheese (full fat => 8%) (natural fat) with 1.5 tsp coconut sugar, to get all the nutrient). In alternance. With a break to avoid the unbalance of the microbiome. One third of the time per type: yogurt, a kind of cottage cheese, nothing (abstinence)
Intersting about coconut sugar , is it really superior than common sugar ? RP mentioned that it causes gas for some people.
Glutenfree diet for several weeks in the past helped me with back pain too, though I can eat gluten now.
Still I get neck pain everytime I eat eggs . Any idea how to increase tolerance to eggs ? -
@Gardner said in My Protocol for Hypothyroidism + Starch/Fat sensitivity:
Intersting about coconut sugar , is it really superior than common sugar ?
=> GI is 55 for coconut sugar, while cane or beet sugar is 70. The last 2 ones are refined, even brown cane because a little molasses has been added (fake). Coconut sugar has a special taste; must be accustomed. Slight caramel taste close to brown cane sugar.
Coco sugar is not suitable for strawberries alone, for example, but it is good if the fruit is accompanied by some type of cottage cheese. Mine is *** and bought by Greenweez.com (in France, coming from Indonesia or les Philippines). Sugar clumps easily. I stir once a week.
Organic coconut blossom sap sugar. So, not refined.

Coco sugar is not suitable for strawberries alone, for example, but it is good if the fruit is accompanied by a certain type of cottage cheese, soft white cheese, 8 % fat).
Don’t trust the seller about a better glycemic index (25 – 35 GI)."Glutenfree diet for several weeks in the past helped me with back pain too, though I can eat gluten now."
=> Even if you don’t perceive it, WGA from wheat has an impact on tight junctions: (it forces the border brush of the intestines to open via the secretion of zonulin). You repair during the night. If you don’t abuse. Everybody won’t react with the same intensity. I’ve already posted a graph here with the standard reaction to the different kinds of gliadin."Still I get neck pain everytime I eat eggs . Any idea how to increase tolerance to eggs ?"
=> You’d better listen to your sensation and not force. Stop 2 months, completely. Then no more than 2 eggs 2x/wk. Try not to get brownish fried eggs when cooked in a pan (adulterated protein) (altered).
If you don’t listen to the message, your body will mark eggs like an an intruder (foreigner). The immune system will rebel. -
@Gardner tolerance to eggs , use raw pineapple with core
-
@sunsunsun said in My Protocol for Hypothyroidism + Starch/Fat sensitivity:
@Gardner tolerance to eggs , use raw pineapple with core
Not practical , everytime I want to eat egg I have to get somewhere pine apple and then juice it ... crazy
No doubt it might work but , don't you get mouth ulcers (canker sore) from eating pineapple ? -
@Gardner then cry
-
@Gardner said in My Protocol for Hypothyroidism + Starch/Fat sensitivity:
@sunsunsun said in My Protocol for Hypothyroidism + Starch/Fat sensitivity:
@Gardner tolerance to eggs , use raw pineapple with core
Not practical , everytime I want to eat egg I have to get somewhere pine apple and then juice it ... crazy
No doubt it might work but , don't you get mouth ulcers (canker sore) from eating pineapple ?raw egg is very allergenic for me.
Anyway, simply frying eggs (at higher temperature than boiling) deactivates most of allergens and makes them much more tolerable. Oxidized cholesterol is small amount is not a big deal