New Therapeutic Strategies for Brain Edema and Cell Injury
2 Bradykinin is a mediator of edema formation
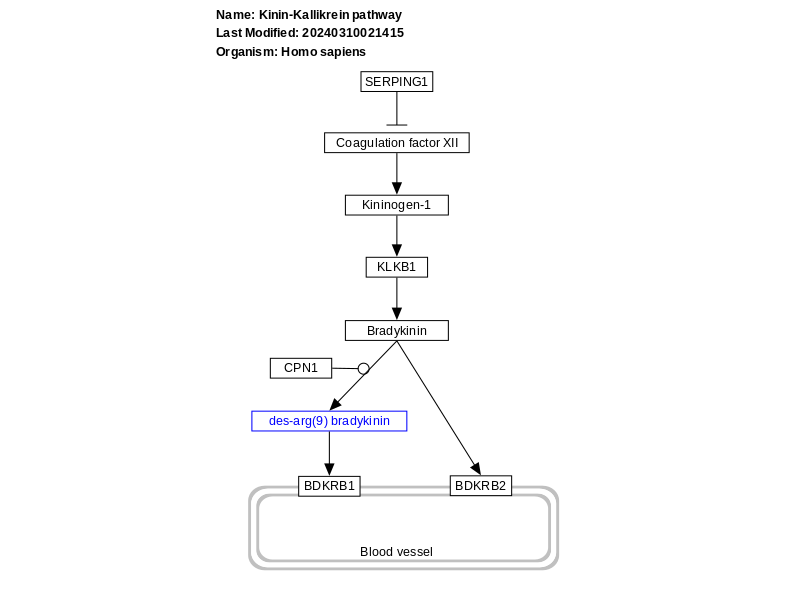
Bradykinin is a well-known mediator of the brain edema formation and BBB disruption (Gröger et al., 2005; Plesnila et al., 2001; Schulz et al., 2000). However, its role in BSCB permeability is still not clear (Bannister et al., 2014; Ma et al., 2019; Mandadi et al., 2016; Pan, Kastin, Gera, & Stewart, 2001; Sharma, 2000; Wahl, Görlach, Hortobágyi, & Benyó, 1999; Xu et al., 2008; Yan-Feng, Gang, & Yan-Ting, 2008). Increased bradykinin content following brain injury has been demonstrated. Bradykinin has 2 receptors such B1 and B2. The detail mechanisms of B1 and B2 receptors in mediating the BBB permeability however, is still not well known (Görlach et al., 2001; Görlach, Benyó, & Wahl, 1998; Görlach & Wahl, 1996; Gröger et al., 2005; Plesnila et al., 2001; Schulz et al., 2000; Schürer, Temesvari, Wahl, Unterberg, & Baethmann, 1989; Unterberg, Wahl, & Baethmann, 1984; Wahl et al., 1996; Wahl, Young, Edvinsson, & Wagner, 1983; Whalley & Wahl, 1983).
Both bradykinin and its receptors are present in healthy human brain and altered in disease processes such as ischemic brain injury (Bannister et al., 2014; Xu et al., 2008; Yan-Feng et al., 2008). Increased bradykinin concentration in the cerebrospinal fluid (CSF) is well documented for traumat6ic brain injury, ischemic stroke and intracerebral hemorrhages (Gröger et al., 2005; Kunz et al., 2013; Ma et al., 2019; Plesnila et al., 2001; Schulz et al., 2000; Schürer et al., 1989;Unterberg et al., 1984; Wahl et al., 1983; Whalley & Wahl, 1983). Increased bradykinin concentration correlates well with the severity of brain edema (Kunz et al., 2013; Unterberg et al., 1984; Unterberg, Polk, Ellis, & Marmarou, 1990; Wahl et al., 1983; Whalley & Wahl, 1983). Brain edema following increased bradykinin concentrations in the brain is largely due to bradykinin-induced vasodilatation together with venous constriction (Unterberg et al., 1984; Wahl et al., 1983; Whalley & Wahl, 1983). Bradykinin also increases microvascular permeability to plasma proteins causing fluid retention and development of cerebral edema (Pan et al., 2001; Sharma, 2000; Xu et al., 2008; Yan-Feng et al., 2008).
Several in vitro studies suggest that blockade of B2 receptors decreases the permeability of isolated cerebral endothelial cells and increased the electrical resistance. (Liu, Xue, Liu, & Wang, 2008; Raslan et al., 2010; Schöller, Feiler, Anetsberger, Kim, & Plesnila, 2011; Trabold et al., 2010). This suggest that blockade of B2 receptors somehow strengthen the endothelial cell permeability (Baethmann et al., 1983, 1988; Wahl et al., 1993, 1988, 1990). There are reports that activation of bradykinin B2 receptors increases the size of the lesion in stroke and enhances BBB breakdown resulting in local neuroinflammation (Görlach et al., 1998, 2001; Görlach & Wahl, 1996; Kunz et al., 2013; Pan et al., 2001; Schürer et al., 1989; Sharma, 2000; Unterberg et al., 1984; Wahl et al., 1999, 1996, 1983; Whalley & Wahl, 1983). Upregulation of bradykinin B2 receptors is seen as early as 2 h after the onset of ischemic stroke that continue to be elevated up to 24 h after the primary insult (Dobrivojević, Špiranec, & Sinđić, 2015; Gauberti, Potzeha, Vivien, & Martinez de Lizarrondo, 2018; Smeda & Daneshtalab, 2017). Interestingly, role of bradykinin and its receptors in SCI are still unclear and require further investigation (see Pan et al., 2001; Sharma, 2000).
2.1 Bradykinin stimulates nitric oxide production
Bradykinin induced vasodilatation is largely caused by endothelial production of nitric oxide (NO) (Genaro, Stranieri, & Borda, 2000; Landmesser & Drexler, 2006). Nitric oxide (NO) is a free radical gas and when produced in vivo could also affect microvascular permeability disturbances and cell injury (Sharma, 1998, 1999; Sharma, Alm, & Westman, 1998; Sharma, Drieu, Alm, & Westman, 2000). Our previous studies show that SCI leads to upregulation of neuronal nitric oxide synthase (nNOS) in the traumatized cord and the adjacent rostral and caudal segments (Sharma et al., 1998; Sharma, Westman, Olsson, & Alm, 1996). Upregulation of nNOS is well known to induce NO production that is responsible for cell injury and microvascular permeability disturbances (Sharma, 1998; Sharma & Alm, 2004; Sharma, Alm, & Westman, 1998; Sharma, Nyberg, Westman, et al., 1998; Sharma et al., 1996). This is further substantiated by our findings that when nNOS antibodies were applied topically over the injured spinal cord, cell changes, edema formation and nNOS upregulation in the spinal cord were absent (Sharma et al., 1996; Sharma, Nyberg, Westman, et al., 1998).
In cell culture studies, bradykinin stimulated nitric oxide production by twofold within 30 min after its application. This NO stimulation by bradykinin is blocked by bradykinin B2 receptor antagonist HOE-140 (Sesti, Martino, Mazzulla, & Chimenti, 2005; Zhang, Nasjletti, Xu, & Hintze, 1998). This observation clearly suggests that bradykinin induced endothelial NO production is mediated by bradykinin B2 receptors.
2.2 Bradykinin B2 receptors in spinal cord injury
Bradykinin is implicated in spinal network, neuropathic pain, rhizotomy, inflammatory hyperalgesia and neuroinflammation in the spinal cord (Bannister et al., 2014; Ma et al., 2019; Mandadi et al., 2016; Pan et al., 2001; Sharma, 2000; Xu et al., 2008; Yan-Feng et al., 2008). Very few report deal with bradykinin in spinal cord injury (Pan et al., 2001; Sharma, 2000). There are reports of significant elevation of bradykinin after experimental spinal cord injury (see Pan et al., 2001). Also interaction of bradykinin with aquaporin4 in spinal cord ischemic injury to the cord was described. (Xu et al., 2008) We reported reduction in BSCB breakdown by B2 receptor antagonist HPE-140 in cord injury indicating involvement of bradykinin in SCI (see Sharma, 2000). However, detailed investigations on bradykinin involvement in SCI require further investigations. With view of bradykinin interacting with dynorphin and nitric oxide in the CNS it is important to understand the modulating roles of bradykinin in SCI that upregulated both nitric oxide and dynorphin after trauma (see Bannister et al., 2014; Sharma, Nyberg, Gordh, et al., 1998; Sharma, Nyberg, & Olsson, 1992; Sharma, Olsson, & Nyberg, 1995; Sharma et al., 1996; Stålberg et al., 1998; Winkler, Sharma, Stålberg, & Westman, 1998).
Peat on Bradykinin
Direct mentions are sparse:
"Bacterial endotoxin increases serotonin release from the intestine, and increases its synthesis in the brain (Nolan, et al., 2000) and liver (Bado, 1983). It also stimulates its release from platelets, and reduces the lungs' ability to destroy it. The formation of serotonin in the intestine is also stimulated by the lactate, propionate and butyrate that are formed by bacteria fermenting fiber and starch, but these bacteria also produce endotoxin. The inflammation-producing effects of lactate, serotonin, and endotoxin are overlapping, additive, and sometimes synergistic, along with histamine, nitric oxide, bradykinin, and the cytokines."
"Y. Kuraishi (2015) said that noradrenaline inhibits pain by inhibiting the release of substance P and glutamate (the excitatory amino acid), and that the suppression of cancer pain results in the inhibition of tumor growth and lung metastasis..., apparently by inhibiting the release of substances from cancer cells (e.g., ATP, endothelin-1, and bradykinin). Things that activate and enliven the patient, and that at the same time decrease pain, seem to be therapeutically appropriate."
A role for bradykinin signaling in chronic vulvar pain
Chronic vulvar pain is alarmingly common in women of reproductive age and is often accompanied by psychological distress, sexual dysfunction, and a significant reduction in quality of life. Localized provoked vulvodynia (LPV) is associated with intense vulvar pain concentrated in the vulvar vestibule (area surrounding vaginal opening). To date, the origins of vulvodynia are poorly understood, and treatment for LPV manages pain symptoms, but does not resolve the root causes of disease. Until recently, no definitive disease mechanisms had been identified; our work indicates LPV has inflammatory origins, although additional studies are needed to understand LPV pain. Bradykinin signaling is one of the most potent inducers of inflammatory pain and is a candidate contributor to LPV. We report that bradykinin receptors are expressed at elevated levels in LPV patient versus healthy control vestibular fibroblasts, and patient vestibular fibroblasts produce elevated levels of proinflammatory mediators with bradykinin stimulation. Inhibiting expression of one or both bradykinin receptors significantly reduces proinflammatory mediator production. Finally, we determined that bradykinin activates NFκB signaling (a major inflammatory pathway), while inhibition of NFκB successfully ablates this response. These data suggest that therapeutic agents targeting bradykinin sensing and/or NFκB may represent new, more specific options for LPV therapy.
Bradykinin in Pain & Inflammation + How to Decrease It
Positive Effects of Bradykinin
Although bradykinin may cause problems, it also serves an important purpose in the body.
Bradykinin protects your heart and your nerves from damage. In the heart, it widens vessels and lowers blood pressure, which prevents heart failure and damage caused by high blood pressure. When the spinal cord or other nerves are injured, bradykinin protects nerve cells and prevents them from dying [15, 16].
1) Heart Health and Blood Pressure
High blood pressure can lead to heart failure. Bradykinin widens blood vessels and decreases blood pressure, which can protect the heart and keep it functioning after congestive heart failure [17, 18].
Doctors often take advantage of the protective effects of bradykinin to help patients with heart conditions. Angiotensin-converting-enzyme inhibitors, or ACEIs, are often prescribed to prevent heart failure in people with high blood pressure. ACEIs stop bradykinin from being broken down, and the increased concentration of bradykinin decreases blood pressure [15, 19].
2) Insulin Sensitivity
Bradykinin makes fat and muscle cells more sensitive to insulin, possibly by increasing the activity of insulin receptors on these cells [20].
Insulin resistance, the condition in which cells are not sensitive enough to insulin, develops before and often predicts type 2 diabetes. Because bradykinin increases the insulin sensitivity of certain cells, it may reduce the risk of developing type 2 diabetes. In turn, drugs which increase bradykinin, such as ACEIs, may prevent type 2 diabetes from developing [21, 20].
 2
1 Votes2 Posts331 Views
2
1 Votes2 Posts331 Views